Category: State 340B PBM Legislation
Nevada lawmakers have unanimously passed and sent to the state’s governor legislation prohibiting pharmacy benefit managers and health insurance carriers from discriminating against 340B covered entities and their contract pharmacies.
The state Assembly voted 42-0 on June 3 and the
…Connecticut will not, after all, be the first state to require 340B covered entities to file reports on their 340B program savings and how they use them, under a bill the state Senate gave final passage to late last night.
…The Iowa Senate last week passed a House-approved bill banning pharmacy benefit manager and payor discrimination against 340B covered entities and their contract pharmacies, including reimbursing the entities at a lower rate than non-340B providers.
The Senate voted 49-1 on
…With just minutes to go in this year’s session, New Mexico lawmakers recently passed a bill to stop pharmacy benefit managers from discriminating against 340B providers including reimbursing them at a lower rate than other providers. Gov. Michelle Lujan Grisham
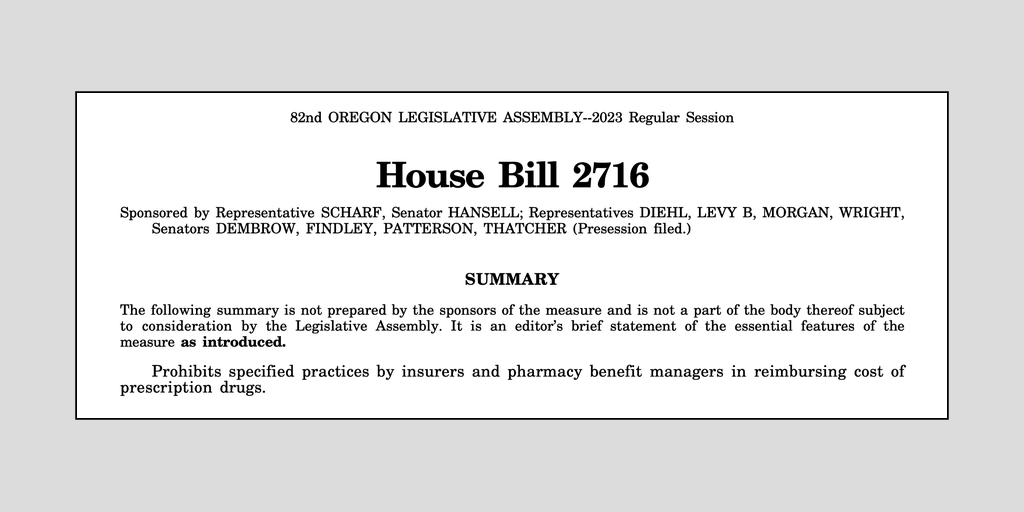
…Oregon legislators have introduced a bill that would prohibit discriminatory practices by pharmacy benefit managers and insurance plans against 340B pharmacies, including reimbursing a 340B pharmacy less for prescription drugs compared with non-340B pharmacies.
If passed later this year, House
…West Virginia has reinforced its groundbreaking 2019 law forbidding what providers say is pharmacy benefit manager discrimination against 340B covered entities.
An amendment passed in March that took effect June 10 clarifies that PBMs or other third-party payers may not require a
…