When Vermont enacted a 340B contract pharmacy access law last week, it also became the first state in the nation [...] …
Category: PBMs and Payers
A major North Carolina health system has sued insurers Aetna Health and Humana for allegedly underpaying for 340B drugs purchased [...] …
News Alert
Rhode Island Senate Passes 340B Contract Pharmacy Access Bill, Vermont Vote Expected Today
The Rhode Island Senate late yesterday unanimously passed a bill to prohibit drugmaker 340B contract pharmacy restrictions, and Vermont state [...] …
President Donald Trump directed his administration Monday to use its trade, regulatory and enforcement powers to establish a “most-favored nation” [...] …
Oklahoma state senators today overwhelmingly passed a 340B contract pharmacy access and pharmacy benefit manager (PBM) “nondiscrimination” bill, sending it [...] …
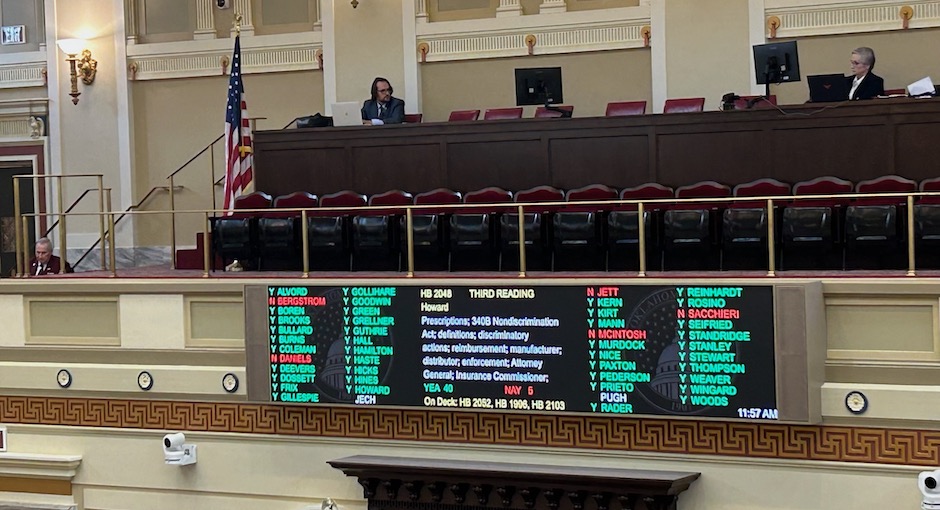
State lawmakers have recently acted on a range of 340B bills in Virginia, Utah and Mississippi as state-level 340B activity [...] …
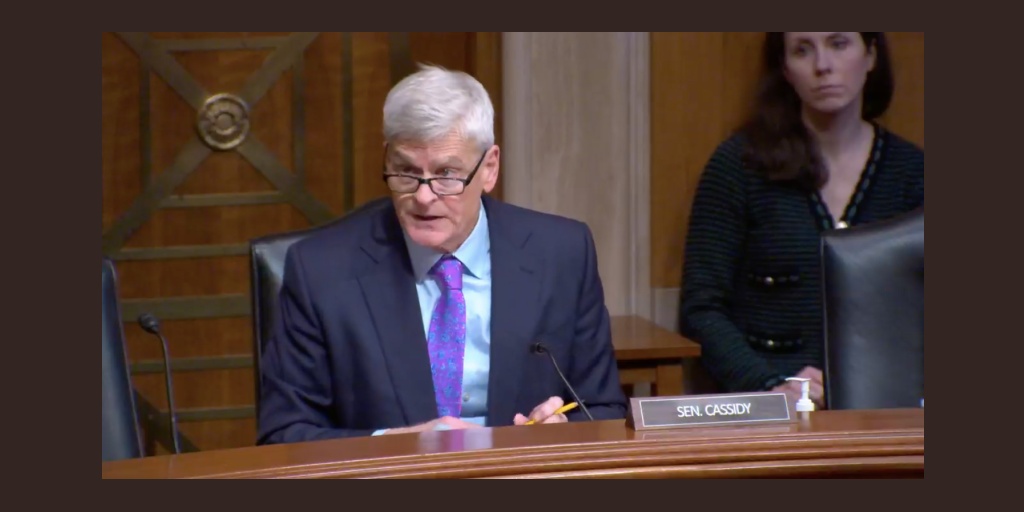
The Republican and Democratic leaders of the U.S. Senate Health, Energy, Labor and Commerce (HELP) Committee—which has jurisdiction over 340B-related [...] …
An influential New Mexico lawmaker is once again pushing to protect state 340B providers from drugmaker contract pharmacy restrictions after [...] …
Federal lawmakers late last week approved a pared-down, must-pass federal spending bill, which cut back on health center funding and [...] …
U.S. House Republican leaders this week unveiled and then quickly backed off of a year-end federal spending package following internal [...] …