Baptist Health of Alabama sued Humana in federal court over the lack of repayment by the company’s Medicare Advantage (MA) [...] …
Category: PBMs and Payers
Missouri state senators in recent weeks have introduced three bills with provisions to bar pharmacy benefit managers (PBMs) from what 340B providers describe as underpayments and other discriminatory practices.
On Jan. 3, Missouri state Sens. Curtis Trent (R) and Doug
…
Eight Mississippi state senators have introduced a bill to bar drugmakers from restricting 340B contract pharmacy use and pharmacy benefit [...] …
A key healthcare committee in the Iowa House of Representatives recently introduced a bill that would bar drug manufacturer restrictions [...] …
Two high-ranking West Virginia state senators recently introduced a bipartisan bill that would prohibit drug manufacturer restrictions on 340B contract [...] …
Rhode Island state lawmakers last week introduced bills that would prohibit both differentiated payments from pharmacy benefit managers (PBMs) to [...] …
Amid expected congressional gridlock, there is a much higher likelihood of state legislative action on 340B contract pharmacies than federal [...] …
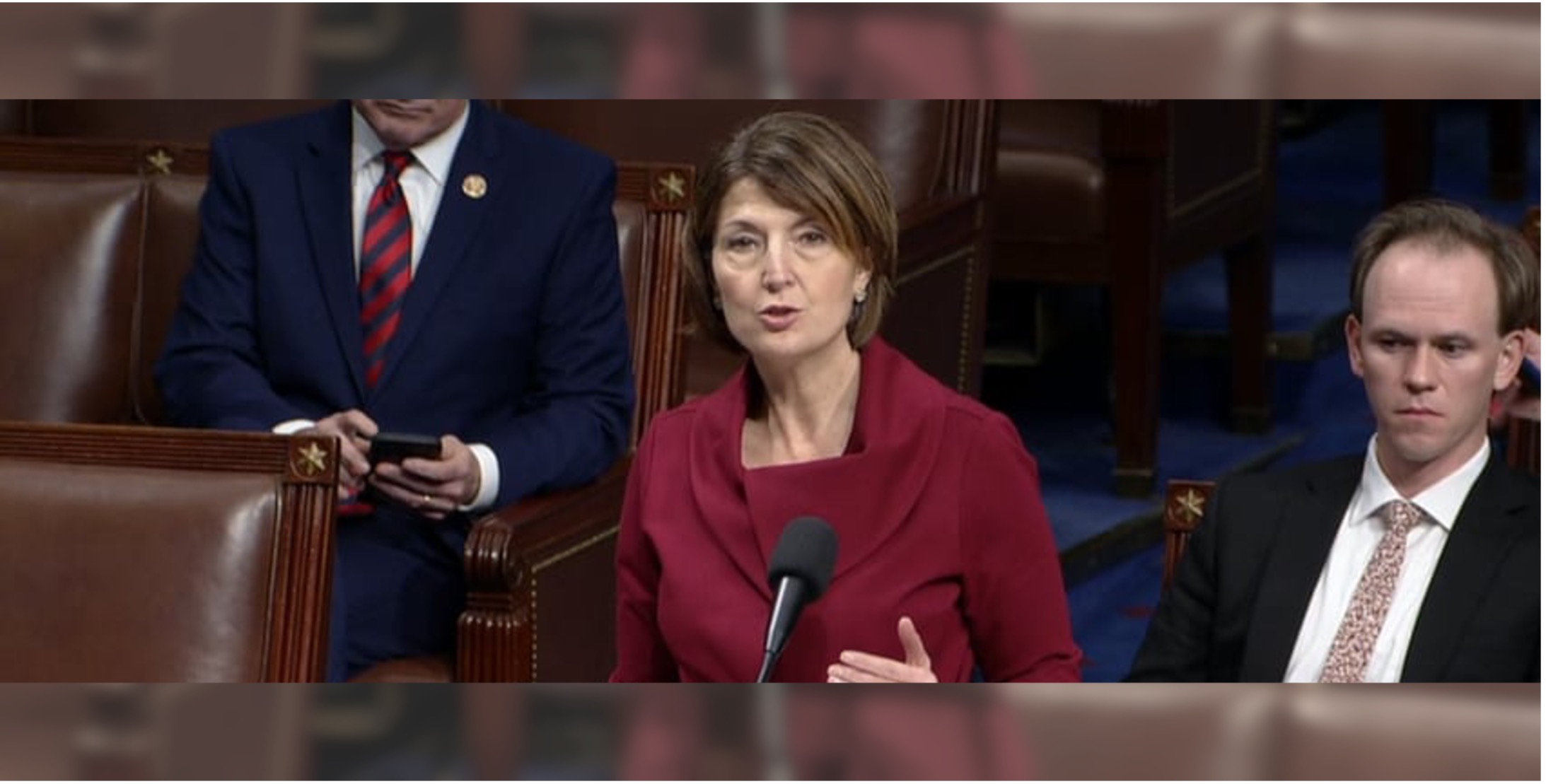
The U.S. House of Representatives last night passed a sweeping healthcare package that would require 340B providers to publicly report [...] …
A Missouri state senator has filed to reintroduce a bill that would bar drugmaker 340B contract pharmacy restrictions and pharmacy [...] …
Just a week after Wisconsin state senators introduced a bipartisan bill to bar disparate treatment of 340B providers by pharmacy [...] …