Category: PBMs and Payers
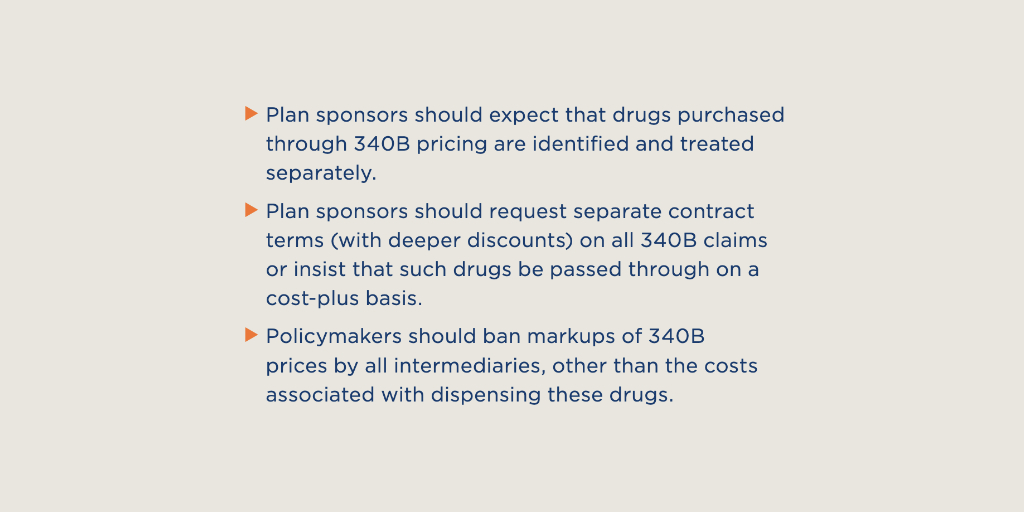
A new “playbook” for employers on getting the upper hand with pharmacy benefit managers says PBM handling of 340B drugs is a top 10 concern for business-sponsored health plans.
Released yesterday by the Washington, D.C., based National Alliance of Healthcare
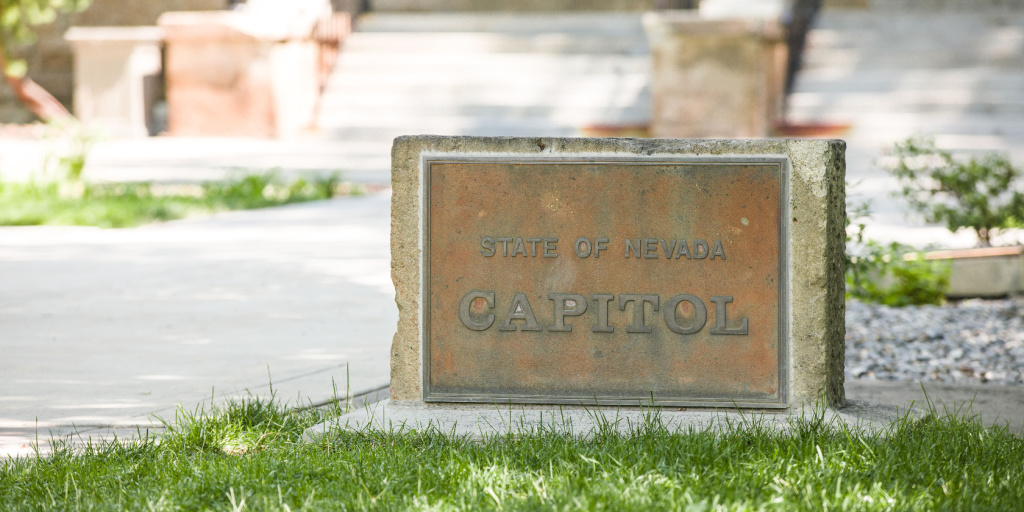
…Nevada lawmakers have unanimously passed and sent to the state’s governor legislation prohibiting pharmacy benefit managers and health insurance carriers from discriminating against 340B covered entities and their contract pharmacies.
The state Assembly voted 42-0 on June 3 and the
…Connecticut will not, after all, be the first state to require 340B covered entities to file reports on their 340B program savings and how they use them, under a bill the state Senate gave final passage to late last night.
…The Iowa Senate last week passed a House-approved bill banning pharmacy benefit manager and payor discrimination against 340B covered entities and their contract pharmacies, including reimbursing the entities at a lower rate than non-340B providers.
The Senate voted 49-1 on
…New Mexico Gov. Michelle Lujan Grisham (D) signed a law April 7 to prevent pharmacy benefit managers and insurers from discriminating against 340B providers. The bill includes language that prohibits payers from reimbursing 340B covered entities at a lower rate
…Two Republican U.S. senators expressed concerns about pharmacy benefit manager encroachment on 340B covered entity savings during a Senate Finance Committee hearing on PBMs last week.
“I often hear concerns from South Dakota hospitals and health centers when it comes
…With just minutes to go in this year’s session, New Mexico lawmakers recently passed a bill to stop pharmacy benefit managers from discriminating against 340B providers including reimbursing them at a lower rate than other providers. Gov. Michelle Lujan Grisham
…