Drugmakers Amgen, GSK, Merck and Sobi recently announced they are exempting more states from their 340B contract pharmacy restrictions amid [...] …
Category: State
Maine recently became the 20th state to enact a 340B contract pharmacy access law as part of a sweeping budget [...] …
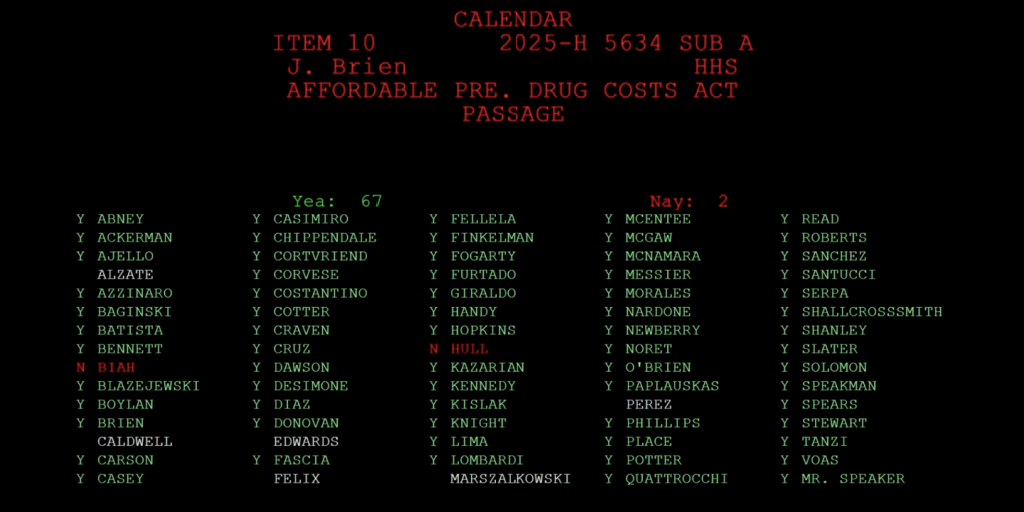
Rhode Island lawmakers wrapped up their 2025 legislative session by passing contract pharmacy access bills that contain provider reporting requirements [...] …
Rhode Island could soon become the next state to pass legislation with 340B contract pharmacy protections and reporting requirements, as [...] …
Maine lawmakers yesterday passed a 340B contract pharmacy access bill that adds new hospital reporting requirements on top of an [...] …
When Vermont enacted a 340B contract pharmacy access law last week, it also became the first state in the nation [...] …
Oregon 340B providers are applauding the state’s new law prohibiting drugmakers from placing 340B contract pharmacy restrictions in the state. [...] …
A U.K.-based drugmaker recently asked a federal court to strike down Nebraska’s contract pharmacy access law, making it the latest [...] …
Vermont and Oregon yesterday became the latest states to enact 340B contract pharmacy access laws, with Vermont’s new statute also [...] …
In the final hour of Oklahoma’s 2025 legislative session, as the clock neared 11 p.m. on May 29, state legislators [...] …