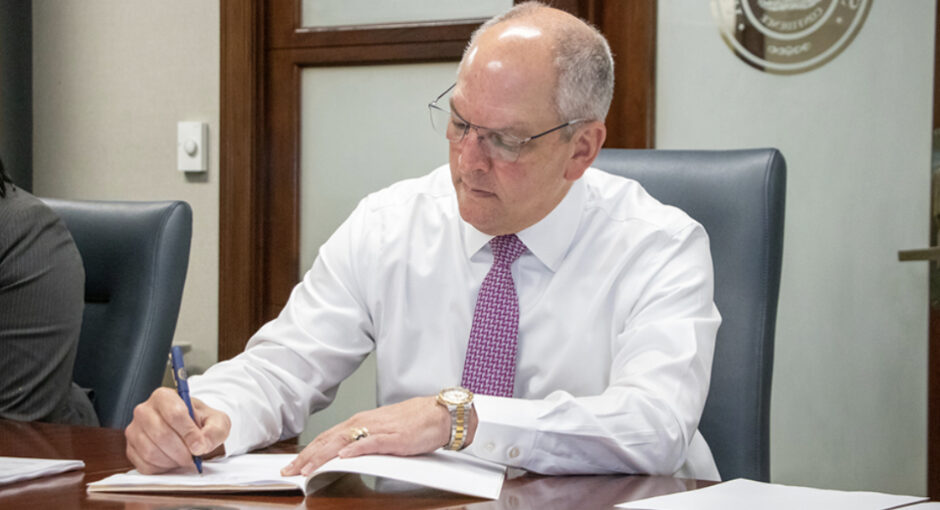
Louisiana Gov. John Bel Edwards (D) has signed legislation making his state just the second with a law addressing manufacturer conditions on deliveries of 340B-acquired drugs to contract pharmacies.
Arkansas’s Act 1103, passed in August 2021, was the first. A federal appeals court is considering its constitutionality. Pharmaceutical Research and Manufacturers of America filed that suit and it is expected to sue to derail Louisiana’s new law.
Edwards signed HB 548, now known as Act 358, on June 12. It prohibits actions by a drug manufacturer or distributor that would deny, restrict, prohibit, or otherwise interfere with the acquisition of a 340B discounted drug to a pharmacy that is under contract with a 340B entity.
It also prohibits practices by a health insurance issuer, pharmacy benefit manager, or other third-party payor that would limit or impose conditions that would indirectly lower the amount of reimbursement for 340B drug dispensed by a 340B entity or its contract pharmacies. A little over half of the states have passed one or more laws since 2019 addressing alleged discriminatory 340B drug reimbursement.
The state House passed the bill 97-2 in late April and the state Senate passed it 38-0 early this month.
In other state 340B legislative and regulatory developments:
Connecticut
Connecticut Gov. Ned Lamont (D) on Wednesday signed a health care cost-containment bill that prohibits PBMs and payers from discriminating against 340B entities. But it does not, as originally drafted, bar drug manufacturers from limiting use of 340B contract pharmacies nor require covered entities to file reports on their 340B program savings and how they use them.
Lamont signed HB 6669, now called Public Act 23-171, on June 21. The state House passed it on June 6 and the state Senate on June 7.
The new law also directs the state Commissioner of Social Services to convene a working group to evaluate and report by Jan. 31, 2024, on:
- the 340B program’s current status
- national efforts to strengthen 340B
- “opportunities for state action to protect 340B revenues of federally qualified health centers from unfair administrative barriers or unnecessary conditions based on such centers’ status as a 340B covered entity.”
Nevada
Gov. Joe Lombardo (R) signed AB 434 into law on June 12. Now called Chapter 390, it prohibits pharmacy benefit managers and health insurance carriers from discriminating against 340B covered entities and their contract pharmacies. It takes effect Jan. 1, 2024. The state Assembly and Senate passed AB 434 early this month.
New York
The chair of the New York state Assembly Health Committee has introduced a bill to prohibit drug manufacturers, PBMs, or any others “from engaging in practices that discriminate against 340B covered entities and their pharmacy partners.”
June 8 was the last day of the state legislature’s 2023 session. Assemblymember Amy Paulin (D) introduced the bill, A7789, on June 15.
It says no entity, including drug manufacturers or PBMs, may
- deny, prohibit, condition, or otherwise limit the dispensing of drugs from a 340B covered entity (the definition of which includes entities’ contract pharmacies)
- deny access to drugs manufactured by a pharmaceutical manufacturer to a 340B covered entity based on such covered entity’s participation in the 340B program
- impose requirements, exclusions, reimbursement terms, fees, audits, claim identification, or other conditions on a 340B covered entity that differ from those applied to entities that do not participate in 340B.
The bill says any contract contrary to these provisions is void and unenforceable. It authorizes the state Commissioner of Health to impose civil monetary penalties on violators.
A bill justification statement on the Assembly website notes that the state on April 1 transferred Medicaid managed drug benefits to Medicaid fee for service, “which will result in hundreds of millions of dollars in lost savings for 340B providers.”
“Both the pharmaceutical industry and pharmacy benefit managers have sought to weaken what remains of the 340B program by imposing arbitrary limitations and requirements designed to enhance their bottom lines,” the statement continues. “These abusive practices include denying required discounts to hospitals and their affiliated contract pharmacies for 340B drugs, requiring labor-intensive ‘tagging’ of 340B drugs, and refusing to distribute 340B
drugs to hospital and contract pharmacies.”
“These actions transfer savings that have been used by safety net institutions to serve vulnerable communities directly into the profit margins of these corporations,” it says. “This bill would prohibit these abusive practices and other attempts to discriminate against 340B providers and ensure that the savings from the 340B program continue to be available to the safety net health care providers in New York State.”
In a related development, two bills that state Senate Health Committee Chair Gustavo Rivera (D) introduced in May to give financial relief to 340B providers hurt by the Medicaid drug benefit transfer did not advance out of committee.
Pennsylvania
The Pennsylvania Department of Health Services has postponed implementing a rule, originally due to start July 1, requiring all claims billed to Medicaid managed care organizations for 340B purchased drugs to include an indicator or modifier showing the prescription was filled with a 340B drug.
Covered entities expressed strong opposition to the requirement during meetings on May 25 and June 15 with state Medicaid officials and in written comments to the department. A state-assembled stakeholder workgroup on how to prevent duplication of 340B discounts and Medicaid rebates on drugs dispensed to managed care beneficiaries is scheduled to meet July 20.