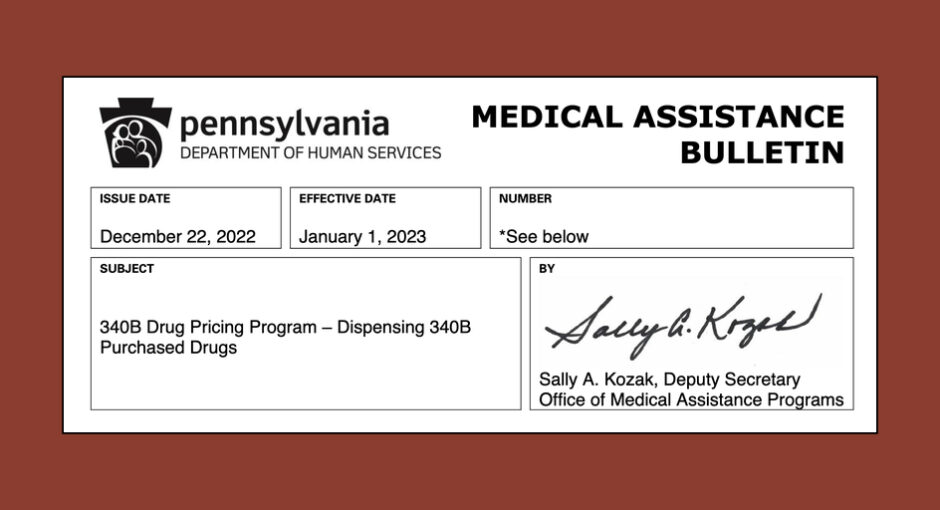
Pennsylvania 340B health centers and hospitals are alarmed about a Dec. 22 state human services department notice to providers that 340B covered entities’ contract pharmacies “must dispense non-340B-purchased drugs to [Medicaid] beneficiaries in the [fee for service] and managed care delivery systems.”
The document had a Jan. 1 effective date and arrived during the holidays when many entity pharmacy staff responsible for 340B were taking time off. It also coincided with a gubernatorial transition, making it hard for about a week to know whom in the department was in charge, entity representatives said. Josh Shapiro (D) was sworn in as governor yesterday, succeeding Tom Wolf (D). Shapiro last week named anesthesiologist Dr. Val Arkoosh to be the new human services secretary. Now serving in an acting capacity, her nomination must be approved by the Pennsylvania Senate.
The state human services department acknowledged but has not yet responded to a request for comment about the bulletin.
“Contract pharmacies generally do not know at the time of dispensing and billing whether a [Medicaid] beneficiary is eligible for 340B-purchased drugs,” the bulletin said. “The [Medicaid] program is unable to identify 340B-purchased drugs dispensed by contract pharmacies, therefore, contract pharmacies must dispense non-340B-purchased drugs to beneficiaries in the FFS and managed care delivery systems. The department invoices drug manufacturers for Medicaid rebates on these drugs.”
“Going to be Catastrophic”
Cheri Rinehart, president and CEO of the Pennsylvania Association of Community Health Centers, said in an interview Friday that PACHC members say “it’s going to be catastrophic” it the change is not delayed.
“Worst case scenario, we need time to decide what services need to be cut and to notify the patients who are counting on those services,” Rinehart said. “Best case scenario, we come up with a more acceptable way to ensure there are no duplicate discounts.”
Rinehart said, and other Pennsylvania 340B stakeholders interviewed confirmed, that an effort was undertaken in the state several years ago to find a different, more acceptable way to identity when contract pharmacies dispense 340B-purchased drugs to Medicaid managed care beneficiaries so the state would not seek rebates on those drugs. Rinehart said the project “stopped on [the state’s] end. Covered entities were more than happy to work with the department to figure out a way, but it was allowed to pretty much die on the vine.”
Rinehart said the state human services department says it believes that the Dec. 22 provider bulletin did not reflect a change in state policy. “However, it’s the first time in writing that the agency has affirmatively prohibited contract pharmacy participation in 340B.” She said a number of Pennsylvania health centers “had sought legal advice and had been told they were within their legal rights to use contract pharmacies” to dispense 340B drugs to Medicaid beneficiaries.
The Dec. 22 bulletin had a dual purposes. One was to announce and implement a narrow policy: a list of nine relatively expensive physician-administered drugs “for which 340B covered entities may only dispense non-340B-purchased drugs to [Medicaid] beneficiaries.” The other purpose was to state a broad policy: that entities’ contract pharmacies must dispense non-340B-purchased drugs to Medicaid fee for service and managed care beneficiaries.
Jolene Calla, vice president of The Hospital and Healthsystem Association of Pennsylvania, said yesterday in a statement: “The Pennsylvania Department of Human Services (DHS) issued a December 22, 2022, Medical Assistance Bulletin (MAB) to update procedures for dispensing 340B-purchased drugs and to implement a 340B Drug Exclusion List. The bulletin applies to Medicaid providers in both the fee-for-service and the managed care delivery systems. DHS says this bulletin further clarifies its existing position relative to contract pharmacies and Medicaid drug rebates; however, hospitals and other covered entities perceive it to be a significant policy change with far-reaching financial implications for some. A meeting has been scheduled with DHS and hospitals to discuss the new MAB in detail.”