Pharmaceutical Research and Manufacturers of America (PhRMA) is seeking a new director for its policy and research team to help develop and lead implementation of work on 340B and related hospital cost and affordability issues, according to an employment solicitation
…Category: Legislative
Maryland Gov. Larry Hogan (R) has signed legislation prohibiting pharmacy benefit manager (PBM) discrimination against 340B covered entities and their contract pharmacies.
Hogan signed HB 1274 into law on May 16. It takes effect Oct. 1. The state House and Senate
…Legislation in Connecticut that would have kept drug manufacturers from imposing “any preconditions, limitations, delays or other barriers” to 340B drug purchases “that are not required” by the 340B statute, died when this year’s legislative session ended on May 4.
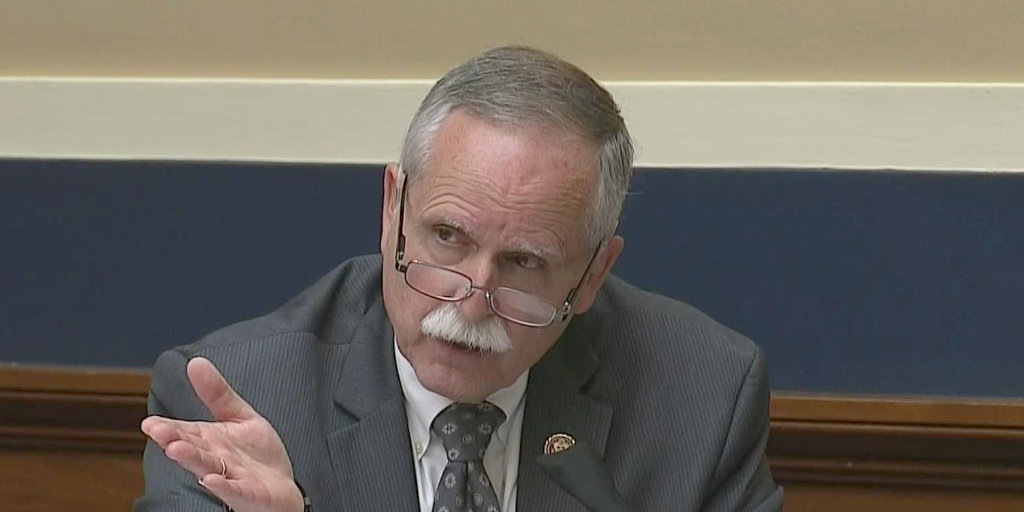
…In a major blow to the 340B provider community, U.S. Rep. David McKinley, the leading voice for the 340B program in the House Republican caucus, was defeated Tuesday in the West Virginia Republican primary. McKinley will remain in office until
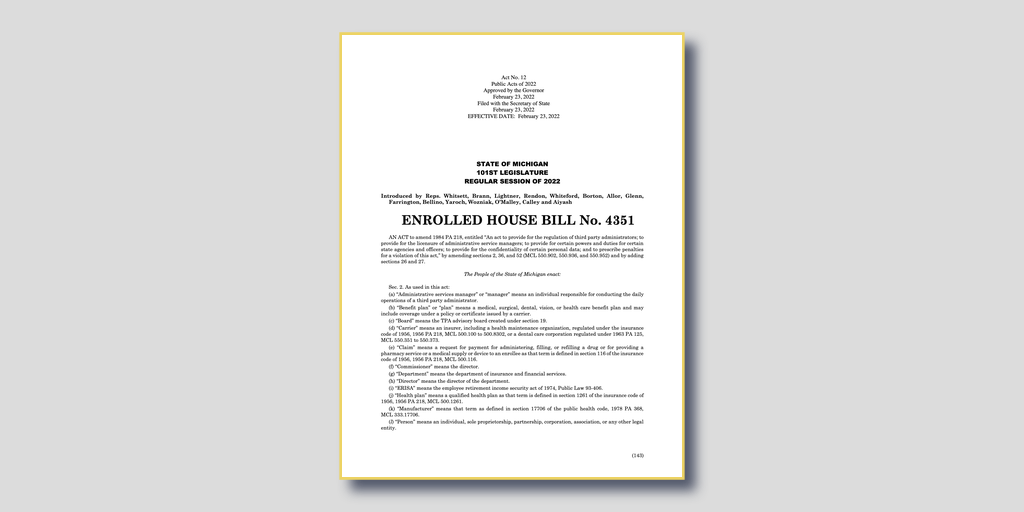
…Drug manufacturers are asking Michigan state legislators to erase language in a new state law that Michigan hospitals say bars the companies from withholding 340B pricing if a covered entity refuses to hand over its contract pharmacy claims data, 340B
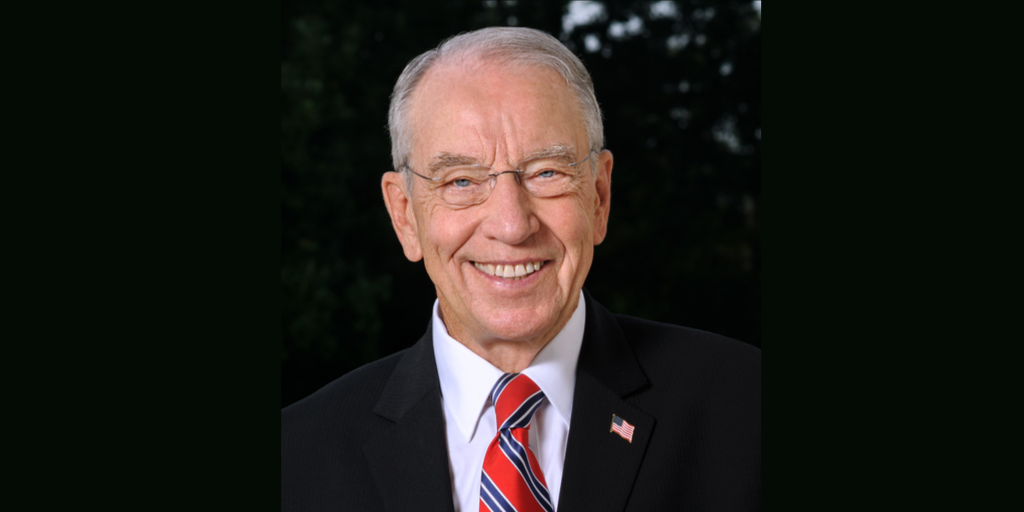
…Senate Finance Committee ranking Republican Chuck Grassley (Iowa) yesterday asked the U.S. Health and Human Services Department of Inspector General (OIG) if it plans to punish seven drug companies over their denials of 340B pricing when hospitals, health centers, and
…Conservative Democratic U.S. Sen. Joe Manchin (W.Va.) has endorsed and appeared in a campaign advertisement for Republican Rep. David McKinley (W.Va.), a moderate being challenged for re-election by a candidate endorsed by ex-President Donald Trump.
The GOP primary between McKinley
…Retired U.S. Sen. Orrin Hatch of Utah, a conservative Republican icon who helped create and shape the 340B drug pricing program, has died. He was 88.
Hatch personally was responsible for choosing one of the 340B program’s most important covered
…