An American Hospital Association senior executive told a U.S. House subcommittee yesterday her group opposes creating “significant new reporting requirements for 340B hospitals that do not reflect the true value or intent of the 340B program.”
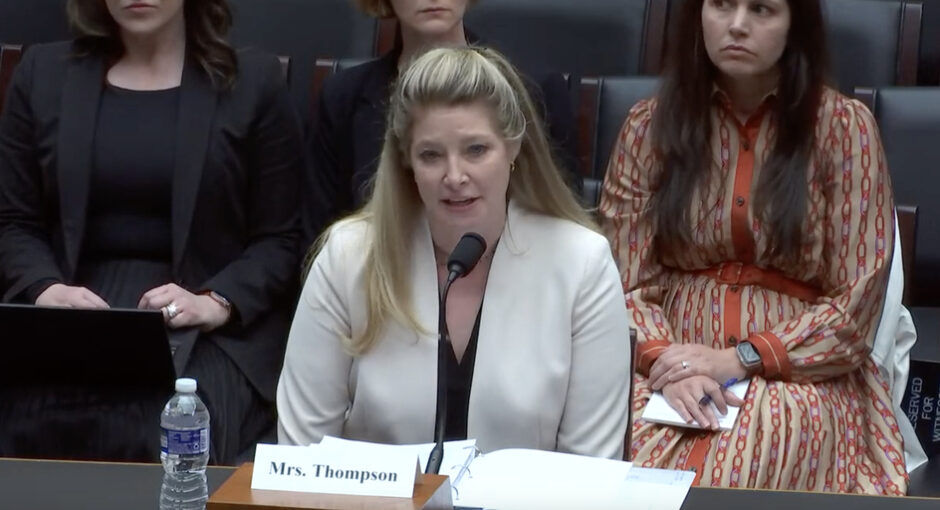
But when asked by a sympathetic lawmaker, Rep. Doris Matsui (D-Calif.), whether AHA could back hypothetical new requirements that do reflect 340B’s actual purpose and value, maybe requirements based on AHA’s own voluntary 340B good stewardship principles for its members, AHA Senior Vice President of Public Policy Analysis and Development Ashley Thompson paused for a moment before answering that it could not.
“I’m just not sure additional reporting requirements are needed at this time,” Thompson said.
The House Energy & Commerce health subcommittee held yesterday’s hearing to discuss 17 actual and draft bills that its Congressional sponsors believe would bolster transparency and accountability in health care. Those measures include subcommittee Vice Chair Larry Bucshon’s (R-Ind.) draft bill to impose new reporting requirements on disproportionate share hospitals and potentially other covered entities as well.
Some 340B program veterans say persuading hospitals to accept new 340B reporting requirements is the key to passing long-sought federal legislation that validates contract pharmacy use in 340B, ends pharmacy benefit manager encroachment on providers’ 340B savings, and creates a neutral third-party drug claims clearinghouse to protect manufacturers from paying duplicate 340B discounts and Medicaid rebates on the same drugs.
Thompson’s testimony indicates that America’s biggest hospital group does not appear to be budging on the issue for now.
She said focusing tightly on statistics such as “payer mix at every single clinic” that uses 340B-purchased drugs, as Bucshon’s bill would, “will mask all the good work that’s being done from the program.”
“It will be very difficult to identify, for example, that a hospital is using the savings to hire behavioral health specialists to work in an opioid clinic, or to provide free or discounted drugs to needy patients, or to provide a mobile mammography unit,” Thompson said. “I’m not sure that metrics” like those Bucshon wants “will really be able to show the good works that are being done right.”
“OK, so what kind of [reporting] could we support that would not be captured by the requirements in this bill?” Matsui asked Thompson.
“You really need to reflect on additional reporting requirements because there’s so many already on hospitals,” Thompson said. “I really do feel that HRSA has the authority to make sure that the program is being implemented as intended. It audits hospitals to make sure that they’re conforming to the program as written.”
In her written testimony, Thompson noted that 340B hospitals already “must annually recertify their eligibility to participate and attest to meeting all the program requirements; participate in audits conducted by HRSA and drug manufacturers; and maintain auditable records and inventories of all 340B and non-340B prescription drugs.” During questioning, she pointed out that hospitals also report data to the Centers for Medicare & Medicaid Services and to the Internal Revenue Service that is relevant to their participation in 340B.
“340B hospitals are committed to transparency, but believe transparency should involve mutual concessions,” Thompson said. “Any measures that increase transparency for 340B providers also should include greater transparency for drug companies, including how they set their prices and how much they decide to increase their prices.”
CEO, COO, CFO, and Janitor
Matsui asked Thompson if adding 340B reporting requirements would “be workable for hospitals, especially rural hospitals and others with limited resources.”
“You’re absolutely right,” Thompson said. At many small rural hospitals “the CEO is also the COO, the CFO, and the janitor who changes the light bulb. So any additional requirements, you hope that they’re not so high a barrier that it decreases the ability of providers to access the funds that might be available.”
Rep. Bill Johnson (R-Ohio) said although the 340B program is a lifeline to hospitals in his “very rural district,” he is “getting increasingly concerned that some nonprofit 340B hospitals are abusing the program rules to actually deprive patients of the types of support that 340B was intended to provide.”
“Many of our largest hospital systems, beneficiaries of the 340B program, complain about the cost of price transparency compliance,” Johnson said. “And yet they have signed an HHS Health Sector Climate Pledge to, among other things, designate an executive level lead for their work on reducing emissions by 2023, and to conduct an inventory of emissions by the end of next year.”
“I’m not sure how this relates to delivering affordable quality healthcare, but it sounds awfully expensive to me,” he said. “I find it hard to believe that some hospitals complain that they’re unable to shoulder the burden of transparency that they say costs too much, yet they can afford the not-so-little cost of climate resilient infrastructure.”
“I’m just not sure there’s not abuse here,” Johnson said.
In his prepared testimony, hearing witness Brian Connell, executive director of federal affairs at the Leukemia & Lymphoma Society, said his group is “encouraged that the committee is considering program reforms aimed at understanding how patients receiving care at 340B facilities are benefiting from the significant drug discounts provided to those facilities.”
“We agree that the 340B program should be the subject of additional scrutiny to better determine how to best achieve its goals of promoting patient access to necessary treatments,” he said. “We urge the committee to continue to consider 340B program reforms that would improve transparency around how covered entities utilize the significant discounts they receive under the program, in order to promote the sharing of these discounts with patients served by these facilities.”
Buschon Presses CMS Administrator on Part B Reimbursement
Subcommittee Vice Chair Bucshon did not bring up his draft 340B transparency and oversight bill during the hearing. He did, however, address hospital participation in 340B from a different angle.
He asked CMS Administrator Chiquita Brooks-LaSure, the lead witnesses at the hearing, why CMS is not using its controversial 2020 survey of 340B hospitals’ acquisition costs for drugs reimbursed by Medicare Part B as the basis for determining hospitals’ Part B reimbursement for such drugs. Hospitals panned the quality of the survey and its timing which occurred just as the COVID-19 pandemic began to surge. Hospital groups also questioned the survey’s legality.
Brooks-LaSure noted that the Trump administration decided to lower hospitals’ Part B reimbursement for 340B-purchased drugs from the default average sales price plus 6% payment rate to ASP minus 22.5% and the Biden administration reversed the decision. Bucshon pointed out that the current administration was doing so because the U.S. Supreme Court ruled in June 2022 that the cuts were unlawful.
Although CMS under President Trump surveyed hospitals about their 340B acquisition costs for Part B drugs, it decided against setting 340B hospital’s Part B drug reimbursement on the basis of the survey.
In September 2022, a federal district judge ordered CMS to immediately begin paying hospitals at the default ASP plus 6% rate for the remainder of 2022. In January, the same judge ruled that the underpayments from 2018 to 2022 were illegal but he did not order CMS to repay hospitals immediately.
About a week before he ruled, CMS said on a government website that it would issue a proposed rule this month regarding “potential remedies” for the underpayments. CMS said in November in its hospital outpatient prospective payment system final rule for 2023 that it would publish the proposed rule about repayments in advance of issuing its OPPS proposed rule for 2024. CMS normally publishes its OPPS proposed rule for the coming year in July. Last week, it sent its OPPS proposed rule for 2024 to the White House for clearance to be published.
During yesterday’s hearing, Bucshon asked Brooks-LaSure when CMS planned to announce how it will handle repayments from 2018 through September 2022.
“We plan to issue it very soon,” she said.