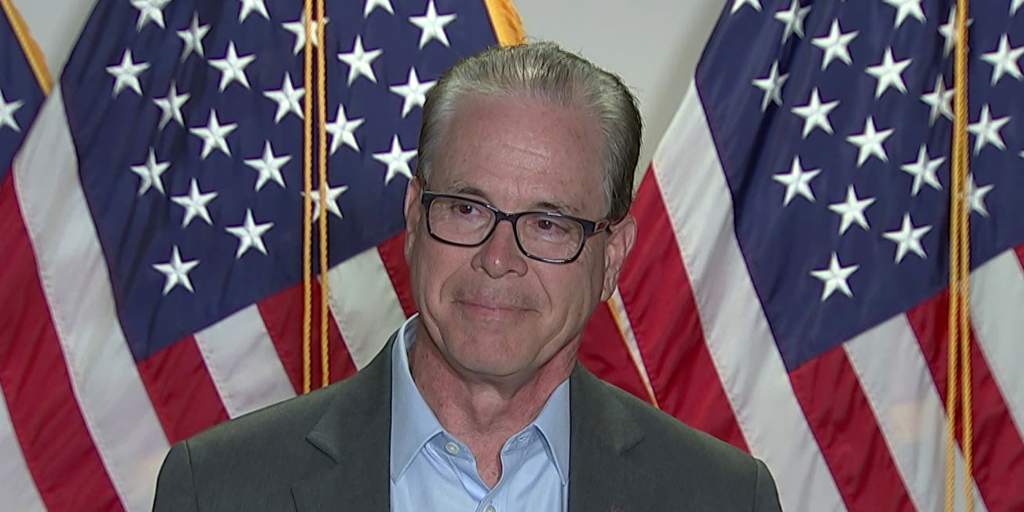
U.S. Sen. Mike Braun’s (R-Ind.) bill would impose reporting requirements on 340B DSH, children’s, and free-standing cancer hospitals and require federal watchdog agencies to issue three reports on the drug discount program | Source: C-SPAN
U.S. Sen. Braun Introduces Bill to Collect and Report 340B Hospital Data
Updated Thursday Nov. 5, 2020, 5:50 p.m. EST to clarify that the bill was introduced Oct. 5 and the text was published on Congress’s official website today. U.S. Rep. Bruce Westerman (R-Ark.) recently introduced the same bill (H.R. 852), with Reps. Tim Burchett (R-Tenn.), Denver Riggleman (R-Va.), and Lloyd Smucker (R-Penn.) as original cosponsors.
U.S. Sen. Mike Braun (R-Ind.) has introduced legislation to require 340B disproportionate share (DSH), children’s, and free-standing cancer hospitals to report data from their main and child sites on patient insurance status, charity care costs, and aggregate acquisition costs and reimbursements for 340B drugs. Congress.gov, the official website for U.S. federal legislative information, published the bill text this morning; Braun introduced the measure Oct. 5.
Braun serves on the Senate Health, Education, Labor, and Pensions Committee (HELP) Committee, which has direct oversight over the 340B program. Since the Senate is expected to remain in Republican control, his legislation is likely to get extra attention as the committee begins to address the program in 2021.
Under Braun’s bill, DSH, children’s, and free-standing cancer hospitals would have to report “the name of all third-party vendors or other similar entities that the covered entity contracts with” for 340B program services. When they enroll in 340B and annually thereafter, DSH hospitals would have to submit “the contract that is the basis for eligibility” to the U.S. Health and Human Services Department (HHS) for review.
The 340B provisions are in Braun’s bill S. 4796, which broadly addresses the costs of health care services, prescription drugs, and health insurance coverage. The bill’s 340B reporting requirements would take effect 14 months after the law’s enactment. Braun’s bill would instruct HHS to issue regulations to carry out the 340B provisions.
HHS’ Health Resources and Services Administration (HRSA) would have to make the hospitals’ patient insurance status, charity care cost, and contract information publicly available on the 340B Office of Pharmacy Affairs Information System (340B OPAIS). The HHS Office of Inspector General (OIG) would have two years from the bill’s enactment to report to Congress on 340B DSH, children’s, and free-standing cancer hospitals’ and their child sites’ provision of charity care. The U.S. Government Accountability Office (GAO) would have one year to report to Congress on 340B DSH hospitals’ contracts with state and local governments to serve low-income patients ineligible for Medicaid, the amounts of care the hospitals must provide under their contracts, and how the contracts define who is a “low-income individual.” GAO would have two years to deliver a report on the difference between 340B DSH, children’s, and free-standing cancer hospitals’ aggregate 340B drug costs and revenues, broken down by child site.
Another section of Braun’s bill would require 340B DSH hospitals to submit and regularly update data, for themselves and their child sites, on their “low-income outpatient utilization rate” for the most recent fiscal year. The section defines “low-income outpatient utilization rate” the same as the Social Security Act’s definition for purposes of Medicare DSH adjustment payments, except with references to “inpatient” switched to “outpatient” and other comparable changes, and the definition expanded to include child sites. HRSA would have to report this data to Congress annually.
Braun’s bill comes on the heels of HELP Chair Lamar Alexander (R-Tenn.) and U.S. House Energy and Commerce (E&C) ranking Republican Greg Walden’s (Ore.) call for ideas on how 340B could be improved (see story below). It could be the first of several bills to alter 340B introduced during the lame duck session.
Groups representing 340B hospitals probably will object strongly to the bill. Groups representing other 340B covered entities probably will criticize the bill for overreaching and express concerns that Braun’s proposed requirements will eventually apply to them.
Braun represents Indiana, where Eli Lilly and Co. is headquartered. Lilly has stopped providing 340B pricing on its products shipped to contract pharmacies, except for one contract pharmacy per covered entity for those lacking an in-house pharmacy, and now requires covered entities to charge patients no more than 340B cost for its insulin products and to not charge a dispensing fee.
340B Will Get More Scrutiny from Congress in 2021
As we went to press, neither President Trump nor Democratic candidate Joe Biden appeared to have won the 270 electoral voted needed to win the presidency. Most news organizations and pollsters agree that Biden is leading Trump in the electoral count.
Despite defending more seats than Democrats, Republicans appeared to be holding on to their majority status in the U.S. Senate. Democrats appear to have suffered a net loss of between three and five seats in the U.S. House, another surprise. Even with that erosion, the party is still in the majority in the chamber.
The following observations are partially derived from a memorandum written by 340B Report sponsor Powers Law not yet widely available.
Rep. Frank Pallone (D-N.J.) will likely remain as chair of the House Energy and Commerce Committee (E&C), which has jurisdiction over the 340B program. 340B covered entities consider him to be a strong ally. In September, he, Health subcommittee chair Anna G. Eshoo (D-Calif.), and Oversight and Investigations chair Diana DeGette (D-Colo.) wrote to U.S. Health and Human Services (HHS) Secretary Alex Azar to express “strong concerns” about several drug manufacturers’ recent moves to stop providing 340B pricing on drugs shipped to contract pharmacies, or to condition continuation of such pricing on provision of claims data.
Rep. Greg Walden (Ore.), E&C’s ranking Republican member, is retiring. Reps. Michael Burgess (R-Texas), Cathy McMorris Rodgers (R-Wash.), and Bob Latta (R-Ohio) are vying to succeed him. Burgess, as Health subcommittee chairman during the 115th Congress, held hearings on 340B, and he and others introduced bills aimed mostly at increasing oversight over 340B hospitals, reducing their access to 340B discounts, and scaling back 340B contract pharmacy. McMorris Rodgers has supported the 340B program in the past, but has not been active in 340B affairs for several years. Latta has not been active on 340B.
Sen. Health, Education, Labor, and Pensions (HELP) Chair Lamar Alexander (R-Tenn.) also is retiring. The committee oversees the 340B program. Sen. Michael Enzi (R-Wyo.) is in line to succeed him, but he too is retiring. Sens. Richard Burr (R-N.C.), Rand Paul (R-Ky.), Susan Collins (R-Maine), and Bill Cassidy (R-La.) are next in seniority. Cassidy, as a senator and before that as a representative, has paid close attention to 340B. His HELP Act during the 115th Congress would have placed significant restrictions on 340B hospitals. If Cassidy succeeds Alexander, expect the HELP Committee to pay much more attention to 340B. Any Senate legislation that would put major restrictions on the 340B program likely would get a cold shoulder from the Democratic-controlled House.
Sen. Mike Crapo (R-Idaho) will succeed Sen. Chuck Grassley (R-Iowa) as Finance Committee chair because Grassley is term-limited. The committee has jurisdiction over Medicaid and Medicare. As a senior committee member, Grassley will stay involved in the 340B debate.
HIV/AIDS Clinics Pitch Neutral 340B Duplicate Discount Clearinghouse Idea
Congress should eliminate duplicate 340B discounts and Medicaid managed care rebates on the same drugs by creating a neutral, third-party clearinghouse to identify and remove 340B claims from state rebate requests in a confidential manner, HIV/AIDS clinics told two Republican congressional committee leaders last week.
Congress also should prohibit discriminatory reimbursement against 340B covered entities by pharmacy benefit managers (PBMs) and other third-party, for-profit payers “that are unregulated in the 340B stakeholder program and were never the intended beneficiaries of the program,” Ryan White Clinics for 340B Access (RWC-340B) said in comments to U.S. Senate Health, Education, Labor, and Pensions (HELP) Chair Lamar Alexander (R-Tenn.) and U.S. House Energy and Commerce (E&C) ranking Republican Greg Walden (Ore.).
The lawmakers—both retiring in early January—invited 340B stakeholders last month to submit ideas on how to improve the drug discount program. Last Friday was the deadline. The two lawmakers haven’t disclosed their next steps. They might introduce legislation, but the odds of passage during a lame duck session are slim.
On Tuesday, we covered what groups representing drug manufacturers, health systems and hospitals, and community health centers floated to Alexander and Walden.
RWC-340B said preventing duplicate 340B discounts and Medicaid rebates, and protecting 340B covered entities from discriminatory reimbursement, are the “two issues that we believe require immediate congressional action and/or intervention.”
Regarding 340B duplicate discounts on Medicaid managed care claims, it said it has shared draft legislative language with House Energy and Commerce Committee and Senate Finance Committee staffers. RWC-340B says giving the task to a neutral third party would “introduce fairness and protection of sensitive information to the end goal.”
“Because the neutral third party would protect the confidentiality of the information, all stakeholders would be protected from any potential misuse of their information,” it said. “The idea of such a federal structure and oversight of duplicate discounts is not a new one, it simply takes on new significance” in light of drug manufacturers’ unilateral denials of 340B pricing on drugs for contract pharmacies, which the manufacturers say “are intended to prevent duplicate discounts.”
Regarding ending discriminatory 340B drug reimbursement, RWC-340B said the practice “ultimately harms the low income and medically vulnerable patients served by 340B providers.” PBMs and private, for-profit payers are usurping 340B program savings covered entities use “to treat more vulnerable patient populations or to improve services for them,” it said.
The National Association of Community Health Centers (NACHC) made a similar case about the need to address 340B “pick pocketing” in its comments to Alexander and Walden.
RWC-340B challenged Alexander and Walden’s statements, made in their invitation for 340B reform ideas, that 340B program changes are overdue, and that a lack of data hampers 340B oversight. It said those characterizations of 340B are “unfair an inaccurate.”
“The conversation we should be having is how we can all work together to protect the 340B program” from drug companies’ denials of 340B pricing for prescriptions filled by contract pharmacies, and drug companies’ efforts to change 340B from an up-front discount program to a rebate model, it said.
Ex-HHS OIG Senior Policy Analysts’ Comments
Alexander and Walden also got comments from Madeline Wallack and Suzanne Herzog, the principals of Rx|X Consulting. In the early to mid 2000s, Wallack and Herzog led influential studies of 340B for the U.S. Health and Human Services Department (HHS) Office of Inspector General. Congress included many of their 340B program integrity recommendations in the Affordable Care Act.
Wallack and Herzog, as did RWC-340B and NACHC, told Alexander and Walden “there must be reimbursement protections for 340B entities so that the savings are not appropriated to insurance companies and PBMs.” They also said “covered entities need protections surrounding fair contract terms and fee schedules from pharmacies and other vendors” in the 340B contract pharmacy space. “While there are a range of issues across all vendors, we are seeing more aggressive terms from specialty pharmacies, especially when the pharmacy is owned by a PBM,” they said.
Wallack and Herzog also said:
-
The U.S. Centers for Medicare & Medicaid Services’ (CMS) nearly 30 percent reduction in hospitals’ Medicare Part B reimbursement for 340B-purchased drugs “does not address the issue of rising drug costs and has no impact on the manufacturers. It only harms 340B hospitals.”
-
Across states, policies for preventing 340B duplicate discounts are inconsistent. Within states, policies often are vague or limited. The U.S. Health Resources and Services Administration’s (HRSA) Medicaid exclusion file—its tool for communicating covered entities’ 340B billing strategies for Medicaid fee for service to the states—does not apply to contract pharmacy. “CMS and HRSA must work together to develop a new tool with better technology,” Wallack and Herzog said.
-
Manufacturers propose solving their duplicate discount problem by requiring covered entities to hand over 340B contract pharmacy claims data, so it can be cross-checked for overlapping Medicaid, Medicare Part D, and commercial rebate claims. Wallack and Herzog said they suspect the “real issue” for manufacturers is PBM “stacked rebates”—the fact that, when a PBM owns a 340B contract pharmacy (especially when it owns a contracted specialty pharmacy), “the pharmacy typically charges a percentage of the margin on the payment they also set as the payer. They then still collect the PBM rebate.” Wallack and Herzog said “it would be wise to address [this issue] directly,” rather than hold covered entities hostage “to the problem of confusing payer contracts/PBM rebates.”
-
HRSA should be auditing the accuracy of inputs to the calculation of the 340B ceiling price, Wallack and Herzog said. HRSA also should routinely review the impact of “prior period adjustments” that manufacturers make on calculations of the components of the 340B ceiling price up to three years post-submission. When these adjustments lower 340B ceiling prices, covered entities should get refunds, they said.
-
Congress should reverse the exclusion of 340B pricing on orphan drugs for rural and free-standing cancer hospitals. “What was the point of adding rural provider types to the list of 340B eligible entities when they cannot benefit from the much-needed discount on the most expensive drugs?” Wallack and Herzog asked.
Hospital Association Comments
America’s Essential Hospitals’ and Catholic Health Association’s (CHA) main points to Alexander and Walden were aligned with other hospital groups’ points: 340B discounts are “indispensable” and “critical” to their members; drug manufacturers are violating the 340B statute in ways that harm hospitals, but legislation isn’t necessary; and Congress should use its oversight power to stop manufacturers’ 340B program abuses.
Both associations raised manufacturers’ denials of 340B discounts on drugs delivered to contract pharmacies, and efforts to replace up-front 340B discounts with back-end rebates. America’s Essential Hospitals said the U.S. Centers for Medicare & Medicaid Services’ (CMS) deep cuts in Medicare Part B drug payments to 340B hospitals “not only…hamstring essential hospitals’ ability to execute the 340B program as Congress intended but…restrict patient access to needed therapeutics and cost taxpayers more over time.”
“While legislative action is not needed, there is a role for Congressional oversight to ensure that the Department of Health and Human Services (HHS) is enforcing the drug manufacturers’ obligations under the law,” CHA said.
America’s Essential Hospitals said “fundamental reforms to the program are unnecessary.” Congress instead should “use its oversight authority to ensure the program continues to work as devised.”
Health Center Comments
Piedmont Health and Carolina Health Centers (CHC), federally qualified health centers (FQHCs) with locations across North Carolina (Piedmont) and South Carolina (CHC), submitted comments echoing those made by the National Association of Community Health Centers (NACHC). They said:
-
Redefining 340B narrowly as prescription drug assistance for low-income, uninsured, and underinsured patients would harm FQHCs and their patients.
-
FQHCs need protection from 340B drug reimbursement and contracting “pick pocketing” by PBMs and large for-profit companies.
-
FQHCs could accept an independent third-party claims clearinghouse or other standardized national system to prevent duplicate 340B discounts, but for Medicaid rebates only.
-
FQHC’s ability to contract with multiple pharmacies must be protected.
-
There should not be a one-size-fits-all 340B patient definition. The definition should support the primary care medical home model that underpins FQHC patient care.
-
Letting manufacturers replace prospective 340B discounts with retrospective 340B rebates poses grave risks to FQHCs and should not be allowed.
Administration Wants to Give Most Health Regulations a 10-Year Shelf Life
The Trump administration yesterday proposed to sunset all U.S. Health and Human Services Department (HHS) regulations 10 years after being issued, keeping only those that HHS decides are still needed and have “appropriate impacts.” Rules issued jointly with other agencies, rules that cannot be legally rescinded, and rules pertaining to military, foreign, or HHS internal or personnel matters would be exempt. Comments are due Jan. 4.
The direct impact on the 340B program would be limited. At this time, the HHS secretary has congressional authority to issue 340B program regulations on just three subjects: standards and methods for 340B ceiling price calculations; imposition of civil monetary penalties on drug manufacturers for knowing and intentional 340B overcharges; and establishment of a mandatory and binding 340B administrative dispute resolution (ADR) system. HHS has published final rules for the first two but not the third. HIV/AIDS clinics and community health centers have sued HHS Secretary Alex Azar to force him to issue regulations setting up the ADR system.
HHS yesterday published a notice of proposed rulemaking describing the proposed the 10-year sunset policy for its regulations. If Democratic candidate Joe Biden becomes president, his administration likely would pause and/or withdraw the proposed rule.
The 340B program is administered largely under sub-regulatory guidance. The U.S. Health Resources and Services Administration (HRSA) has asked Congress for years to give it comprehensive regulatory over 340B. It says guidance does not give it “appropriate enforcement capability.”
Last July, HHS created a searchable public database linking to all of its sub-regulatory guidance documents, including those for 340B. All of the database’s pages say the guidance documents “do not have the force and effect of law and are not meant to bind the public in any way.”
In October 2019, President Trump signed an executive order stating that all federal departments and agencies must “treat guidance documents as non-binding both in law and in practice, except as incorporated into a contract,” and “may impose legally binding requirements on the public only through regulations and on parties on a case-by-case basis through adjudications, and only after appropriate process, except as authorized by law or as incorporated into a contract.”
Last month, President Trump signed an executive order that potentially could strip many federal government employees who make policy decisions, including those about the 340B program, of their collective bargaining rights and other federal civil service job protections.
Penn Cancer Docs: Give Private Cancer Clinics Emergency 340B Eligibility
Congress should temporarily extend 340B drug discount eligibility to private oncology practices that care for patients who are newly uninsured or new to Medicaid, and that are located in places where “where there are few cancer care specialists” or where health care markets are “dominated by a small number of large oncology providers,” and three oncologists with joint academic positions at the University of Pennsylvania say.
Doctors Zachary Frosch, Lawrence Shulman, and Justin E. Bekelman outlined their “admittedly provocative” idea in Oct. 22 commentaries published simultaneously in JAMA Oncology and STAT.
Frosch, Schulman, and Bekelman offered a three-part plan to “prevent more closures” of independent oncology practices. First, “we should identify practices whose closure or acquisition is most likely to impair affordable access to cancer care,” they said. Second, “Congress could stabilize these practices’ finances” by “temporarily extend[ing] 340B pricing to [those] that cannot currently qualify.” Third, insurers should pay these practices more per patient if the practices provide “enhanced oncology services” comparable to those under the U.S. Centers for Medicare & Medicaid Services (CMS) Innovation Center’s Oncology Care Model.
The three physicians said extending 340B eligibility to practices “whose closure or acquisition is most likely to impair affordable access to cancer care… might even be consistent with the 340B program’s goal of improving access for the underserved.”
They acknowledged that Congress normally “would be unlikely to enact an expansion of covered entities, but such a radical proposal should at least be considered as an emergency measure to reduce practices’ expenditures and increase their revenue.”
“This measure would be temporary, and the ongoing policy debate about 340B pricing’s pros and cons can be resumed after the crisis,” they said.

