A new study, conducted by L&M Policy Research on behalf of 340B Health, finds hospitals participating in the 340B program treat much higher shares of underserved patients than non-340B hospitals and physicians’ offices. The study was released on July 29.
Researchers examined demographic characteristics of Medicare beneficiaries using 2019 federal data. Specifically, they looked at age, disability status, race and ethnicity, and dual Medicare/Medicaid eligibility of Medicare-enrolled patients of 340B and non-340B healthcare facilities. The study updates an earlier one using 2016 data.
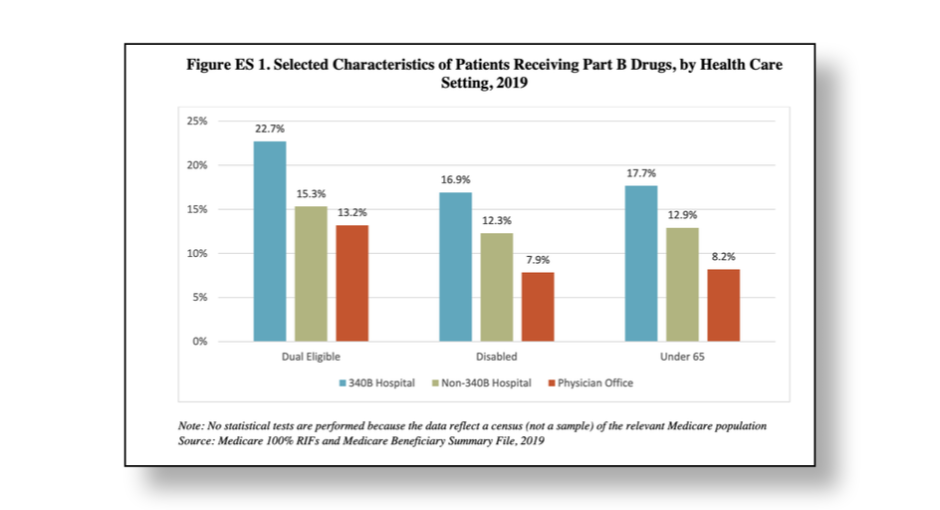
The study found that 340B hospitals serve 48% more patients who are dually eligible for Medicare and Medicaid than non-340B hospitals, and 72% more such patients than physicians’ offices. Dually-eligible beneficiaries must meet very low income and asset thresholds and suffer disproportionately from chronic disease and mental illness requiring more complex, frequent, and costly care. Their low socioeconomic status makes them more likely to experience poor health status and outcomes compared to beneficiaries with Medicare only.
340B hospitals are also more likely to treat patients with Medicare who are under 65, the 340B Health-commissioned study found. These patients qualify for Medicare based on a medical or mental health disability severe enough to render them unable to work, or have been diagnosed with a severe, debilitating diseases such as kidney failure requiring dialysis or amyotrophic lateral sclerosis (ALS). Due to their high level of medical and/or mental health needs, these patients typically require complex and costly care. 340B hospitals treat 37% more Medicare patients under 65 than non-340B hospitals, and 50% more such patients than physicians’ offices, according to the study.
In addition, the study found that 340B hospitals serve 69% percent more Black patients than non-340B hospitals and 63% more than physicians’ offices. Due to longstanding racial health inequities, Black patients are less likely to have access to routine, preventive medical care and bear a higher burden of chronic disease on average than white patients. As a result, they are more likely to require aggressive and costly medical intervention than their white peers.
“Patients who are most in need are much more likely to rely on 340B hospitals for their care, and those hospitals use their 340B savings to provide additional services and reduce inequities in care,” said Maureen Testoni, president and CEO of 340B Health, as quoted in the study news release. “By doing so, 340B serves as a cornerstone in the continuing effort to build more access and equity into the health care system.”
The findings from the 340B Health-commissioned study paint a much different picture of the behavior of 340B hospitals than another recent study commissioned by PhRMA and conducted by the Center for Public Health Law Research at Temple University’s Beasley School of Law. The Temple Law study looked at the financial assistance and debt collection practices of 340B hospitals and found the former to be opaque and highly variable and the latter harsh and aggressive. Based on these findings, The PhRMA-funded study suggested there were “limitations” in 340B hospitals’ use of 340B savings to help patients.
The newly-released study commissioned by 340B Health represents the latest shot fired in an ongoing battle between 340B hospitals and the drug industry over the extent to which 340B hospitals are helping the underserved and are making good use of 340B savings.