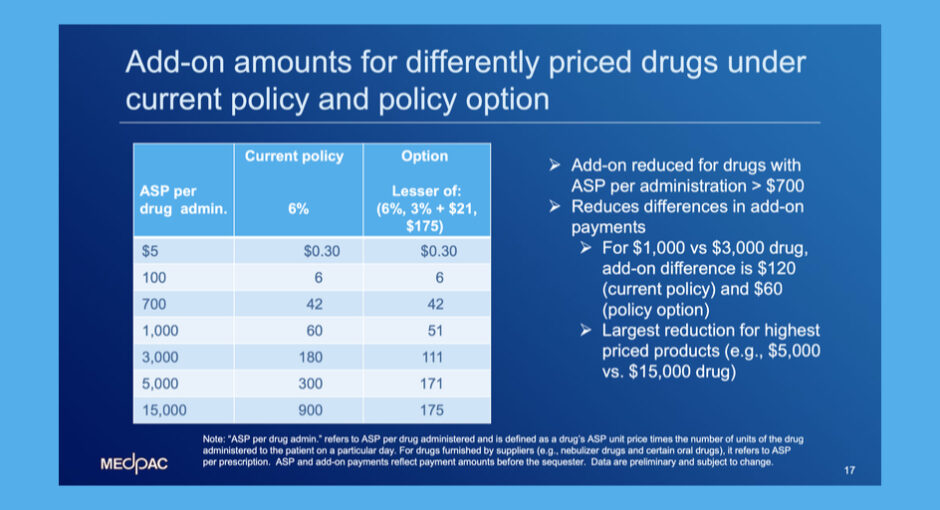
Congressional Medicare advisers are weighing whether to recommend converting the 6% add-on to Part B drug reimbursement to a fixed fee capped at $175 for drugs that cost $15,000 or more, phased in starting with drugs costing above $700.
Medicare Payment Advisory Commission (MedPAC) staff members briefed commissioners during MedPAC’s Sept. 2 meeting about their analysis of the proposed Part B add-on payment change and other ways that Medicare could address the high prices of drugs covered under Part B.
Under a Part B reimbursement option that MedPAC’s staff modeled for the commission, the add-on would stay ASP plus 6% for drugs that cost less than $700 a day to administer.
For drugs that cost between $700 and $15,000, the add-on payment would be the lesser of
- 6%
- 3% plus $21
- $175.
For drugs that cost more than $15,000, the add-on would be a flat $175.
MedPAC’s staff gave these examples of the add-on rate under ASP plus 6% versus the reduced add-on rate:
- for drugs ASP $1,000: $60 add-on now, $51 add-on under proposed policy ($9 less)
- for drugs ASP $3,000: $180 add-on now, $111 add-on under proposed policy ($69 less)
- for drugs ASP $5,000: $300 add-on now, $171 add-on under proposed policy ($129 less)
- for drugs ASP $15,000: $900 add-on now, $175 add-on under proposed policy ($725 less).
MedPAC’s staff estimated that there would be a 2.6% reduction in Part B drug payments overall if the add-on reduction were in place.
In its June report to Congress, MedPAC discussed how Part B drug payments could be adjusted to (1) arrest high launch prices for new “first-in-class” drugs that have limited clinical evidence, (2) encourage price competition among drugs with similar health effects, and (3) decrease financial incentives for providers to use higher-priced drugs.
The third category is probably the one that’s most sensitive now to 340B hospitals.
Until 2018, Medicare paid all hospitals in the outpatient prospective payment system (OPPS) average sales price plus 6% for drugs reimbursed under Part B. From 2018 through the present, Medicare has slashed reimbursement for hospitals’ 340B-purchased drugs to ASP minus 22.5%.
National hospital groups sued CMS for the cuts, and in June the U.S. Supreme Court held that the cuts imposed in 2018 and 2019 were illegal. Hospital groups and the federal government are back in federal district court over the legality of the cuts from 2020 to the present and whether the cut for this year should be stopped immediately.
Estimates of 340B hospitals’ losses range from $1.6 billion when the cuts began to between $1.9 billion and $2.3 billion now.
The reduced 6% add-on payment that MedPAC is considering recommending would apply to 340B and non-340B hospitals alike. For it to take effect, Congress either would have to pass a law or CMS would have to find a way to implement it in an administratively acceptable manner to a federal court—something CMS was unable to do regarding the payment cut for 340B hospitals.
If the new proposed payment reduction were to happen soon, it would be a tough pill to swallow for 340B hospitals. Having just won in court over the payment cut from ASP plus 6% to ASP minus 22.5%, their Part B drug reimbursement rate once again would be lower than it was before 2018. It’s also possible they would not yet have been fully repaid for their five years of losses under the lower payment rate.