SPONSORED CONTENT
Part 2 of 2: Navigating staffing shortages, unpredictable demand, and complex industry requirements
While in-house pharmacies offer a wide array of benefits both for the community health center (CHC) and their patient populations, overseeing the myriad of administrative, operational, financial, and regulatory intricacies can prove difficult to manage. In Part 1 of this series, we covered two of the biggest challenges that CHCs face while operating in-house pharmacies: managing costs and ensuring favorable contracting.
In this follow-up, we explore the pressures facing CHCs due to pervasive staffing and retention challenges, fluctuating levels of patient demand, and nuanced regulatory complexities—and how CHCs can act to boost patient demand, improve clinical outcomes, and reinforce their financial health in 2024 and beyond. This is part two of a two-part series.
Challenge 3: Staffing shortages
Attracting and retaining pharmacy talent has been a challenge for the past several years, as high-traffic, long hours, and high-demand have placed an undue burden on pharmacy staff. This pervasive issue is impacting pharmacy opening hours and their ability to provide patient care across the board: a 2022 National Community Pharmacists Association survey reported that more than 75% of pharmacies were struggling to fill open positions.[1]
For covered entities looking to balance operating costs with patient care, partnering with a third-party pharmacy services manager can make all the difference. These experienced organizations specialize in recruiting talent that will be the best fit for your organization, and oversee onboarding, credentialing, managing staff, help to standardize processes, workflows, and ensure a high level of quality service.
Challenge 4: Improving access to care, health outcomes, and capture rates with CPAs
To meet changing demand, health center pharmacies will need to prepare staff for expanding roles that assist care teams. There are a wide array of services pharmacists may be able to perform as extensions of the care team, including: collaborative drug therapy management, medication therapy management, test and treat, point of care testing and the measurement of other biomarkers to evaluate the therapeutic effects of the drug therapy. Additional services that the pharmacy team can execute include patient assessments, medication adherence initiatives for chronic conditions such as diabetes or asthma, oversee vaccine clinics, and perform patient educational interventions.
Collaborative practice agreements (CPAs), point of care testing, test and treat, drug therapy management, and other services are paving the way for greater integration of pharmacists into patient care to improve access to services and health outcomes. A CPA is helpful in establishing a set protocol for pharmacist collaboration; it is defined by the Centers for Disease Control and Prevention (CDC) as a “formal agreement in which a licensed provider makes a diagnosis, supervises patient care, and then refers patients to a pharmacist, who is authorized to perform specific care functions.”[2]
When working to define your pharmacy’s CPA, it is mission critical to check local and state laws to ensure compliance:
- First, consider which patient care services your in-house pharmacy would like to offer.
- Next, be sure to understand all local and state laws: Does your state allow pharmacists to perform the services you’ve outlined?
- Third, understand the initial and ongoing investment you’ll make. Identify the costs associated with offering these services: How much will training, additional staffing, billing management services, and marketing fees cost?
- Lastly, outline the business case for your CPA: Are you struggling to meet increased patient demand for access to services? Are you currently able to accept new patients in a timely manner and meet their health care needs? If so, could implementing these services drive additional business and help improve patient outcomes?
To meet changing demand, health center pharmacies will need to have adequate staffing and prepare staff for their expanding roles that assist the care team improve access to care, health outcomes, and their organization’s financial health.
Maxor is here to support changing care delivery models and ensure staff are not only trained, but well equipped and prepared to lead this transition—and ultimately help your center address health disparities, increase access to high-quality care, and even improve time-to-treatment for better outcomes.
Challenge 5: Navigating requirements and earning accreditations.
In-house pharmacy management is a highly regulated field with ever-changing licensing, regulatory and statutory requirements. Ensuring compliance is a full-time responsibility that adds undue pressure to internal teams with many other responsibilities. Oversight in any facet can lead to compliance violations, which may result in federal law enforcement investigations.
Pharmacies’ compliance obligations are dependent on a variety of factors such as the size of the pharmacy and geographic location. The main areas of compliance include DEA compliance, electronic prescription compliance, prescription drug ordering, inventory, record keeping—including the federal Drug Supply Chain Security Act (DSCSA)—prescription dispensing and diversion protection, insurance billing and PBM compliance, Medicare and Medicaid billing, and specialty compliance.[3]
Pharmacies can help ensure compliance by partnering with a pharmacy services manager, like Maxor. With dedicated compliance teams, Maxor ensures a careful review of your pharmacy’s unique compliance needs and generates a customized compliance program with tailored policies and procedures, routine maintenance of auditable records and regular monitoring of upcoming/pending regulatory changes.
Beyond compliance, accreditation signals to the market that your in-house pharmacy consistently meets high standards. Pursuing the right accreditations takes time and strategic perspective, as the ones you select depend on what your organization is trying to accomplish. CHCs can consider pursuing community pharmacy, specialty pharmacy and Medicare’s DMEPOS accreditations, or look at various accrediting bodies such as: the Accreditation Commission for Health Care (ACHC), Joint Commission (JCO), Utilization Review Accreditation Commission (URAC), and Center for Pharmacy Practice Accreditation (CPPA).
Not only does accreditation help ensure your patients can receive the best treatment protocols, but it can also assist your organization in gaining access to limited distribution pharmaceuticals and biologicals. Maxor helps navigate your options to identify the ones that are right for your pharmacy.
Ahead: A New Year for In-house Pharmacy Management
Operating an in-house pharmacy is a complex, but rewarding endeavor for any CHC looking to deliver the broadest range of services that support equitable care access and outcome improvements for their patients. To help safeguard the financial and operational success of your center’s in-house pharmacy in the year ahead, partner with an experienced pharmacy manager such as Maxor, that specializes in boosting revenue, workforce expansion, supply chain and formulary management, and more.
[1]https://ncpa.org/sites/default/files/2022-08/Pharmacy%20economic%20health%20survey%20AUG%2022.pdf
[2] https://www.cdc.gov/dhdsp/pubs/docs/translational_tools_pharmacists.pdf
[3] https://www.natlawreview.com/article/pharmacy-compliance-what-do-you-need-to-know

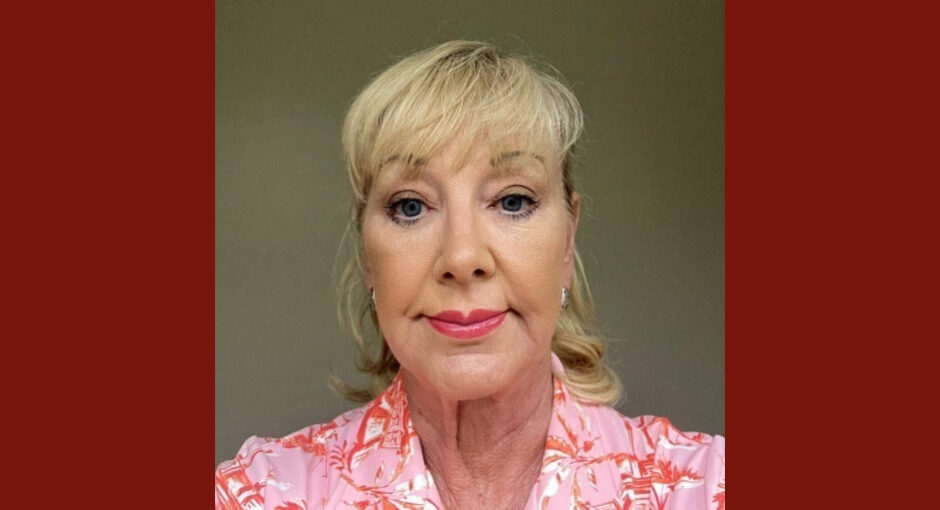
Holly Russo is Senior 340B Director for Maxor. She can be reached at herusso@maxor.com.