More than 1,000 covered entities—double the number in May—are submitting 340B drug claims data to Second Sight Solutions’ 340B ESP platform to be able to keep dispensing manufacturers’ drugs to patients at multiple contract pharmacies, a senior 340B ESP leader said at a major drug industry conference last week.
340B ESP Product Development Lead Andrew Brownlee gave a presentation Friday at Informa’s 2022 Medicaid Drug Rebate Program Summit in Chicago on 340B ESP’s status and what Second Sight and its parent, Berkeley Research Group, have learned and can now predict. 340B ESP Founder and Business Development Lead Aaron Vandervelde gave a similar presentation in May during 340B Report’s inaugural webinar for subscribers about the platform.
In late July, 340B Report published a two-part series on 340B covered entities’ frustrations trying to restore 340B discounts through 340B ESP. It focused on the perspective of 340B providers trying to jump through what appear to be, in many cases, endless hoops to try to restore 340B pricing. At that time, Vandervelde said the slow-downs or breakdowns were largely attributable to the sheer number of stakeholders in the pharmaceutical supply chain and its complexity.
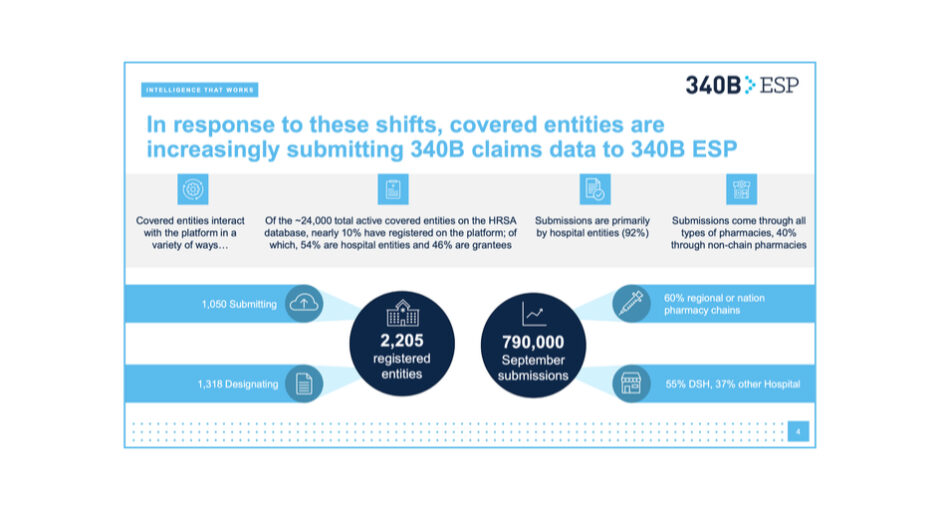
Sixteen of the 18 manufacturers that put conditions on 340B pricing when entities use contract pharmacies use 340B ESP to administer their policies. Just over 2,200 entities are registered on the website, Brownlee said—1,318 to designate a single contract pharmacy to receive 340B-purchased drugs or to claim an exception for a wholly owned pharmacy, and 1,050 to submit claims data to be able to continue dispensing a company’s drugs at multiple contract pharmacy locations.
Entities submitted 790,000 340B claims to 340B ESP in September, Brownlee said. That’s up from the more-than-100,000-submissions-twice-monthly figure that Vandervelde gave in May. Ninety-two percent of submissions are from hospitals, 55% from disproportionate share hospitals alone, Brownlee said. Sixty percent of submissions come through chain pharmacies, he said.
Stakeholders are responding to manufacturers’ conditions on 340B pricing differently, Brownlee said. “After initial opposition, pharmacy chains are supportive of data submission,” he said. Among health plans, “financial losses due to withheld rebates could lead to ‘no 340B’ mandates,” he continued. Payers likewise could try “to narrow contract terms.”
Brownlee said covered entities are responding by interpreting the 340B patient definition more broadly.
“Stemming from the limited, vague language in the initial 340B statute, covered entities and [third party administrators] have now taken control of the patient definition, expanding the ‘eligible’ population of 340B prescriptions,” he said. “This has an effect of not only increasing future 340B utilization but, without a limit on reclassification of historic purchases, leads to large retrospective 340B orders when a covered entity and TPA decide to implement an expanded patient definition.”
Despite manufacturers’ conditions on 340B pricing when entities use contract pharmacies, Second Sight forecasts “continued growth in 340B utilization over the next five years,” Brownlee said.
Total brand drug sales at 340B price now exceed 18%, Brownlee said. Net 340B sales, about $50 billion this year, will approach $90 billion by 2027. “Our forecasting predicts that 340B will be the largest government program, eclipsing Medicare Part D, by 2027,” Brownlee said, with much of the growth coming through expanded 340B purchases of self-administered products.
340B provider groups have raised concerns about potential conflicts of interest with 340B ESP and are urging the passage of the 340B Protect Act which would require the U.S Health Resources and Services Administration to appoint a neutral third party to oversee the claims clearinghouse.