The U.S. Department of Health and Human Services Office of the Inspector General says the Centers for Medicare and Medicaid Services should monitor non-hospital 340B covered entities’ use of modifiers to identify 340B-priced drugs in Part B claims, as these entities get up to speed this year on using the modifiers which will be required for all Part B claims starting January 2024.
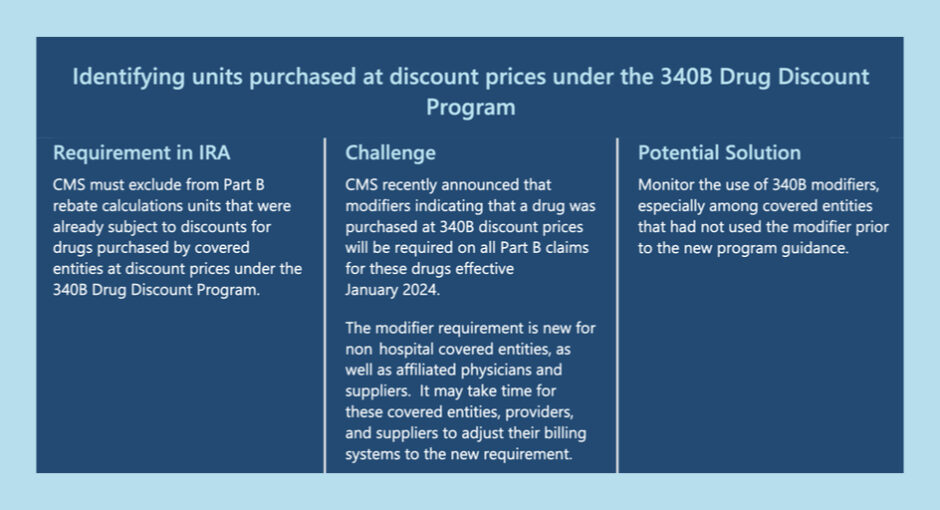
The Inflation Reduction Act allowed CMS to start collecting rebates on certain Part B drug claims, but stipulated that CMS must exclude from Part B rebate calculations drugs that were already subject to 340B discounts.
To that end, CMS issued guidance Dec. 20 requiring all 340B covered entities by Jan. 1, 2024, to use claims modifiers to identify drugs purchased through 340B when they bill for separately payable Medicare Part B drugs.
In a Feb. 7 report, OIG recommended that CMS “monitor the use of 340B modifiers, especially among covered entities that had not used the modifier prior to the new program guidance … For 2023 rebate calculations in particular, CMS may need to take steps to identify claims for 340B-purchased drugs that are submitted without a 340B modifier.”
OIG noted that 340B hospitals have used the modifiers since 2018, but the CMS guidance extended the requirement to include non-hospital 340B covered entities, such as Ryan White clinics and hemophilia clinics, as well as their affiliated providers and suppliers.
“Some of these covered entities, providers, and suppliers may use 340B modifiers for a portion of 2023—or not at all—because the modifier requirement is new for these entities and will require changes to billing systems that could take time to operationalize,” the report said.
Although CMS encouraged non-hospital 340B entities to begin using the modifiers as soon as possible, OIG noted, “For 2023, CMS may not be able to solely rely on 340B modifiers to identify Part B claims for 340B-purchased drugs.”
The report said non-hospital covered entities and their provider and supplier affiliates account for 3% of total associated Part B drug expenditures.
“Had CMS not required modifiers, the agency would not be able to exclude claims for 340B-purchased drugs specifically, and would likely instead need to exclude all claims submitted by covered entities,” the report said. “OIG faced this challenge in previous work and needed to use an extremely burdensome process of matching provider identifiers on Part B claims to the Health Resources and Services Administration’s covered entities database.”
OIG estimated that CMS could have collected $1.4 billion had drug manufacturers been required in 2015 to pay inflation indexed rebates for 64 high-expenditure Part B drugs. “Medicare’s new authority to collect rebates for certain Part B drugs has the potential to recoup billions of dollars for Medicare and its enrollees,” the report concluded.