Although groups representing 340B providers will be measured in any public statements, they are elated by the Democratic sweep of the two U.S. Senate races in Georgia on Tuesday. With Raphael Warnock (D) and Jon Ossoff’s (D) victories, Democrats have taken full control of both chambers of Congress, with very slim margins.
Both parties now have 50 Senate seats, with Vice President-elect Kamala Harris (D) giving her party the majority with her tie-breaking vote. In the U.S. House, Democrats currently have 222 seats to the GOP’s 211, with two vacancies.
While the 340B program has enjoyed strong bipartisan support since its inception, many Republican lawmakers have become increasingly concerned with various aspects of the program. Most of their concerns, which reflect the pharmaceutical industry’s position towards 340B, have focused on program growth, as well as a perception that certain stakeholders, particularly hospitals and large chain pharmacies, are prioritizing profits over patients. The pharmaceutical industry has devoted significant lobbying and public relations resources towards these themes. 340B provider groups have aggressively pushed back and have argued they are using the program as intended.
Under Republican control of the House and Senate, several hearings were held and dozens of bills were introduced to place various restrictions. 340B providers have argued these efforts—focused on narrowing the definition of patient, restricting contract pharmacies, imposing new billing limits, adding reporting requirements, and preventing new hospitals from enrolling in the program—are burdensome and would undermine the program’s purpose.
Democratic lawmakers have largely defended the current structure of the program and have pushed hard against efforts to narrow 340B’s scope. They have also taken an outsized role both at the federal and state level in challenging drug manufacturer efforts to restrict access to 340B pricing at contract pharmacies. With Democratic control of the Senate, the likelihood that U.S. Health and Human Services (HHS) Secretary nominee Xavier Becerra will be approved by the Senate increases significantly. Becerra, currently California’s Attorney General, helped spearhead a bipartisan letter to HHS Secretary Alex Azar demanding the Trump administration take action against the six manufacturers that are no longer allowing covered entities to use the 340B program at their contract pharmacies or are placing restrictions on 340B’s use.
Tuesday’s Georgia runoff results mean Democrats will chair and be the majority parties on House and Senate committees with direct control or significant influence over the 340B program. The biggest changes will be in the Senate, which Republicans had controlled since 2015. Sen. Patty Murray (D-Wash.) will chair the Health, Education, Labor, and Pensions (HELP) Committee, which has primary jurisdiction over the 340B program, succeeding retired Sen. Lamar Alexander (R-Tenn.). Republicans have not yet announced who will be their HELP Committee ranking member. Sens. Richard Burr (R-N.C.), Rand Paul (R-Ky.), Susan Collins (R-Maine), and Bill Cassidy (R-La.) are the senior Republicans, respectively.
Sen. Ron Wyden (D-Ore.) will chair the Finance Committee, which has jurisdiction over Medicare and Medicaid. Sen. Mike Crapo (R-Idaho) is in line to become the committee’s ranking minority member. Under Senate Republican rules, Sen. Chuck Grassley (R-Iowa), who is senior to Crapo, cannot be ranking member in the 117th Congress due to term limits. He is expected to remain on the committee and to continue to be a leading GOP voice on 340B.
In the House, Rep. Cathy McMorris Rodgers (R-Wash.) succeeds retired Rep. Greg Walden (R-Ore.) as ranking Republican on the Energy and Commerce Committee, which has jurisdiction over 340B, Medicare, and Medicaid. Rep. Frank Pallone (D-N.J.) remains chairman.
Rep. Richard Neal (D-Mass.) will continue to chair the Ways and Means Committee, which also has jurisdiction over Medicare. The top Republican is Rep. Kevin Brady (R-Texas).
While much of the early attention of Congress will be focused on the COVID-19 pandemic, don’t be surprised to see inquiries and potential hearings grilling the manufacturer executives who have stopped or limited access to 340B pricing. You can also expect 340B providers will be more proactive in working with their legislative champions to address areas in the program that they believe need improvement. This includes legislation to prevent what 340B providers perceive as discriminatory reimbursement by PBMs and other payors, requiring the government to increase oversight and enforcement of the pharmaceutical industry, increased penalties against manufacturers who they believe are defying the 340B law, as well as a push for more pricing transparency. While 340B providers have welcomed the publication of 340B prices on the U.S. Health Resources and Services Administration (HRSA) Office of Pharmacy Affairs (OPA) web site, they believe that too little information is available for it to be particularly helpful.
The pharmaceutical industry will also work with their champions in Congress, which so far have been almost exclusively Republican lawmakers, to address their perceived flaws with 340B.
Biden Looks To Be on Track to Stop 340B Insulin Rule from Taking Effect
The incoming Biden administration’s decision to immediately halt or delay federal regulations that have not taken effect by Inauguration Day is expected to cover the outgoing Trump administration’s controversial final rule requiring community health centers to pass their 340B program savings on insulin and epinephrine auto-injectors to low-income, uninsured, and under-insured patients.
Biden’s Press Secretary Jan Psaki told reporters on Dec. 30 that the new administration, on the afternoon of Jan. 20, will issue a memo to halt or delay “midnight regulations, actions taken by the Trump administration that will not have taken effect by inauguration day.”
Biden will be sworn in as President on Jan. 20. The 340B insulin rule’s effective date is Jan. 22. The U.S. Health Resources and Services Administration (HRSA) published the rule Dec. 23.
Under the rule, 340B health centers and their subgrantees would have to have written policies and procedures to make insulin and injectable epinephrine available at or below 340B acquisition cost plus a minimal administration fee to patients with low incomes who (a) have a high cost sharing requirement for either insulin or injectable epinephrine, (b) have a high unmet deductible, or (c) have no health insurance. Centers would have to be able to show to HRSA they have such P&Ps to get federal health center program grants under section 330 of the Public Health Service Act.
Health centers say they support making insulin and EpiPens more affordable, but the rule goes about it the wrong way. They say the rule will create substantial new administrative burdens and deprive them of desperately needed revenue during the pandemic. Many patients, they say, could face dramatic changes in how much they pay from insulin from quarter to quarter, or could be shifted from one insulin to another, creating clinical complications.
“We’re hopeful the new administration will prevent any detrimental policies from moving forward,” National Association of Community Health Centers (NACHC) Senior Vice President Amy Simmons Farber said. “We cannot allow any rules or regulations, 340B-related or otherwise, to cause interference or harm to our critical safety net providers. They have been operating on the frontlines of this pandemic since the beginning—and need policies they can rely on to support their efforts, not tie their hands.”
Colleen Meiman, who works for state primary care associations (PCAs) that represent community health centers, said, “We are relieved that the Biden transition team has publicly committed to block all midnight regulations on Jan. 20. This will enable health centers to stay focused on fighting the pandemic, instead of being diverted by the significant administrative and clinical challenges that this misguided regulation would create.”
View From Capitol Hill: An Inside Look at the Latest Developments Shaping the 340B Program
As 340B covered entities continue to feel the financial impact of Medicare Part B reimbursement cuts and drug manufacturer actions that limit access to 340B pricing, a new Administration and new Congress will soon be in place. What will this mean for the future of the 340B program?
Join Omnicell for a live virtual event, “View from Capitol Hill: An Inside Look at the Latest Developments Shaping the 340B Program,” to hear from multiple 340B stakeholders in a lively discussion of the latest industry and legislative developments in 340B—just as the 2021 legislative season gets underway. The session will address:
- The status of proposed and pending legislative and legal actions
- Financial implications from Covid-19 loss of business
- A covered entity’s perspective around strategies for optimizing program performance amidst the ever-changing 340B landscape
- The future of the 340B program
This live session takes place on Wednesday, Jan. 27 from 10:00 AM–11:00 AM PT | 1:00 PM–2:00 PM ET, and will feature Omnicell 340B’s Jeff Spencer; Ted Slafsky, publisher and CEO of 340B Report; Shrujal Patel, co-founder and managing director of Alinea Group, LLC; and a covered entity guest.
Spots are limited, so register today.
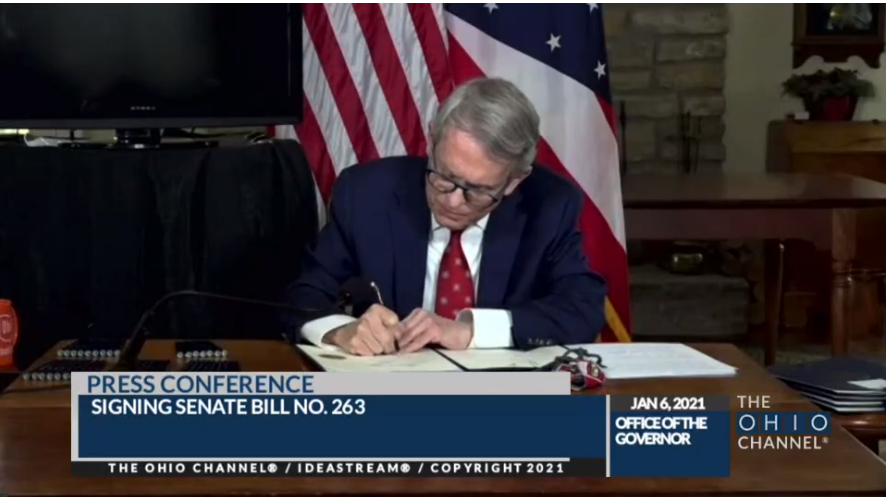
Ohio Governor Signs Bill Stopping Discriminatory 340B Drug Reimbursement
Ohio Gov. Mike DeWine (R) yesterday signed bipartisan legislation that prohibits private insurers, Medicaid managed care organizations, and their pharmacy benefit managers (PBMs) from including provisions in their contracts with 340B entities that would deny them the financial benefit of participating in 340B.
Reimbursement could not be lower than National Average Drug Acquisition Cost (or wholesale acquisition cost if NADAC is unavailable), and payers could not impose fees on 340B entities that are not imposed on other providers or that are higher than those imposed on others. Nine states have passed similar legislation during the past two years, including Utah, Oregon, West Virginia, Minnesota, South Dakota, Montana, Massachusetts, and Rhode Island. Georgia previously was the most recent to do so, in late June.
“Thank you, Governor, for protecting all 340B providers from discriminatory contracts by PBMs,” state Sen. Bob Hackett (R), the legislation’s main Senate sponsor, said during the virtual signing ceremony. “This bill will protect the savings meant to remove barriers to access to quality health care for Ohioans.”
“This legislation ensures our most vulnerable populations have access to medically necessary medications,” said Julie DiRossi-King, Chief Operating Officer for the Ohio Association of Community Health Centers. “[It] levels the playing field by putting protections in place so 340B can function and actually serve those intended; which leads to the right kind of care, at the right time, and in the appropriate, most cost-effective setting.”
PhRMA and Members Signal Fight Against 340B Contract Pharmacy Will Go on
Pharmaceutical Research and Manufacturers of America (PhRMA) says it will keep pursuing contract pharmacy-related and other changes to the 340B program, notwithstanding the U.S. Health and Human Services (HHS) Dec. 30 legal opinion casting doubt on the legality of some PhRMA members’ steps to rein in contract pharmacy in the drug discount program.
Shortly after we published Tuesday’s edition of 340B Report, PhRMA responded to our request for comment on the HHS General Counsel’s advisory opinion. The drug industry association said:
PhRMA continues to have concerns with the growing role of contact pharmacies in the 340B program and the lack of evidence that patients are benefiting from contract pharmacy participation in 340B. It is alarming that outdated guidance that has no basis in the law has enabled for-profit corporations to profit from a program meant to support safety-net facilities and needy patients. PhRMA remains committed to pursuing changes in the program that ensure our discounts help low income and uninsured patients, not contract pharmacies.
Sanofi, one of the six manufacturers that have stopped or imposed conditions on 340B discounts for contract pharmacy drugs, told us in response to the HHS opinion that “often patients receive no discount at all on contract pharmacy-dispensed drugs.” Novartis told us, “The unfortunate reality is that the overwhelming majority of discounts from medicines dispensed at pharmacies are not shared with patients. These discounts benefit for-profit pharmacies, third-party administrators, other midddlemen and hospitals with no requirement that those funds be used for charitable care at hospitals.”
No other manufacturers denying 340B pricing on contract pharmacy drugs responded to our request for comment on the advisory opinion.
Eli Lilly told Modern Healthcare (subscription required), “We’ve reviewed the statement from HHS and we disagree with their conclusion. We continue to believe our 340B distribution program complies with all applicable laws and regulations, and we will continue to advocate for fixes to 340B that will help people access affordable medicines instead of padding the bottom lines of hospitals and contract pharmacies that pocket discounts for themselves.”
AstraZeneca told Modern Healthcare, “We changed our approach to help mitigate the significant compliance issues that have been well documented in audits performed by GAO [the U.S. Government Accountability Office] regarding contract pharmacy arrangements. AstraZeneca’s approach to contract pharmacy arrangements fully complies with all operative requirements and continues to support the mission of the program to provide a healthcare safety net for the most vulnerable patients in our country.”
Frequent 340B Hospital Critics Slam Health System’s Debt Collection Practices
A New York Times article this week about a health system suing patients during the pandemic over unpaid medical bills prompted frequent critics of 340B hospitals to observe that the system has hospitals and offsite outpatient locations enrolled in 340B.
The Jan. 5 Times article said nonprofit New York-based health system Northwell Health “sued more than 2,500 patients last year, records show, a flood of litigation even as the pandemic has led to widespread job losses and economic uncertainty.” The newspaper said about 50 New York hospitals have sued patients over medical debt since last March, mostly smaller facilities upstate.
Among Northwell’s 23 hospitals, Long Island Jewish Medical Center and Lenox Hill Hospital are enrolled in 340B. The Times article did not address Northwell’s involvement in 340B.
Nationally, other health systems with 340B hospitals have drawn national media attention in recent years for their medical debt collection practices, including UVA Medical Center in Virginia, Methodist Le Bonheur Healthcare and Ballad Health in Tennessee, SSM Health (which operates in four states), and Heartland Regional Medical Center in Missouri.
Like this week’s article in the Times, the other articles did not bring up the other health systems’ participation in 340B. Critics of the 340B program have brought it up, however, and the connection is becoming a talking point in arguments for scaling back 340B for hospitals.
We reached out to Northwell for comment about the Times article, its provision of uncompensated care, and its participation in 340B. Modern Healthcare (subscription required) reported yesterday that a Northwell spokesperson said the system “paused legal filings from April through September, and has decided to extend that given the resurgence in COVID cases. That’s in addition to rescinding any legal claims filed in 2020.”
“In the rare instances (less than 0.1 percent of claims) that Northwell is compelled to take legal action, it is only when a patient has been unresponsive to multiple attempts to resolve the outstanding balance and if it is determined that the patient has a strong ability to pay,” the spokesperson said.
“Someone please tell me how a hospital w/ huge #340B discounts can aggressively go after patients. Why aren’t the 340B profits helping these patients in need?” tweeted Ted Okon, executive director of Community Oncology Alliance (COA), about Northwell Health. COA represents private oncology practices.
“Ludicrous!” tweeted Drug Channels blogger Adam Fein, another frequent critic of 340B hospitals. “Purportedly “non-profit” @NorthwellHealth sued 000s of low-income & indigent patients – and only stopped after @nytimes article.”


