As California’s Medicaid program moves toward implementing a fee-for-service payment structure for drug coverage, one of the primary foes of the transition has returned to court to obtain a temporary restraining order.
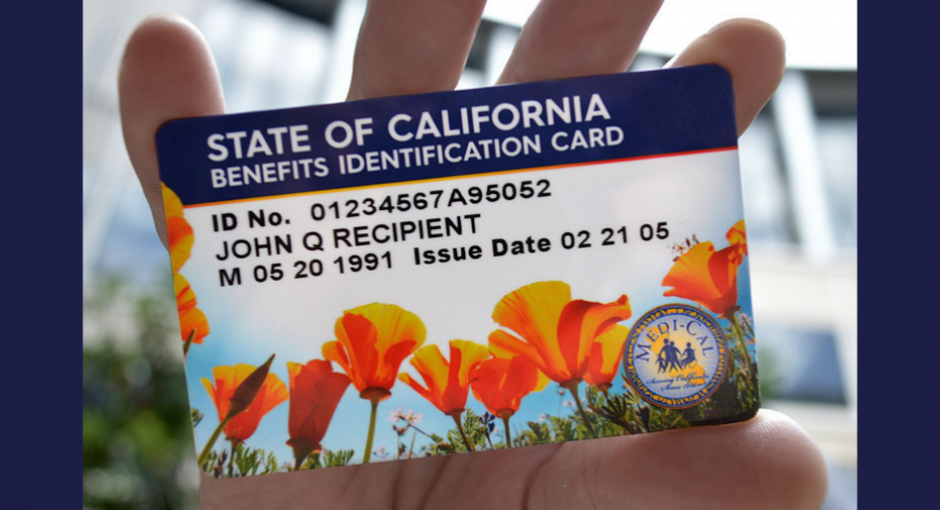
The new Medi-Cal Rx program is intended to save money for California’s Medicaid program, which insures one out of three of the state’s residents. But by requiring 340B covered entities to bill Medi-Cal at acquisition cost for 340B purchased drugs, the policy is expected to deprive 340B covered entities of revenue critical to sustaining their operations.
Officials with the Community Health Center Alliance for Patient Access (CHCAPA) said the state’s plan to transfer Medi-Cal managed care drug coverage to Medi-Cal FFS on Jan. 1, 2022, could cost covered entities between $200 million and $300 million a year in lost 340B revenue. Covered entities currently bill Medi-Cal FFS at acquisition cost for 340B drugs, but they bill Medi-Cal managed care organizations at higher negotiated rates.
CHCAPA represents numerous federally qualified health centers in California that treat more than 2 million patients. It attempted to block the transition by suing in federal court in October 2020, but a judge ruled that the litigation could not proceed until the U.S. Centers for Medicare & Medicaid Services approved the state’s application for a waiver from federal Medicaid policy to make the change.
The San Diego-based organization told U.S. District Judge John Mendez in a Dec. 12 court filing it expects CMS will approve the waiver before the Jan. 1 Medi-Cal Rx implementation date. Because the window of time until Jan. 1 is shrinking, CHCAPA told Mendez, “it is no longer possible to file a regularly noticed motion before January 1, 2022.”
“Given the immediate and irreparable harm that Medi-Cal Rx will cause plaintiffs and their patients, plaintiffs expect to seek a temporary restraining order on shortened time to enjoin implementation of Medi-Cal Rx in the event it is approved by CMS,” the group said.
“It’s imperative that the state be prevented from taking actions that will jeopardize the health of millions of Californians,” CHCAPA President Anthony White said in a recent statement. “We need a solution that will ensure that the drug discount savings remain with community health centers, not the state.”
But as of mid-week, CHCAPA said it cannot yet move forward until the Centers for Medicare & Medicaid Services approves a waiver for the program.
“CHCAPA is prepared to move forward with planned legal action but due to the court’s earlier order cannot take these steps until CMS approves the Medi-Cal Rx transition…which has not yet occurred,” the organization told 340B Report.
Meanwhile, the state Department of Health Care Services, which operates the Medi-Cal program, has posted numerous notices on its website that the transition remained on scheduled for Jan. 1. Its most recent notice, posted on Dec. 9, noted that Medi-Cal Rx would begin processing claims beginning 6 a.m. on New Year’s Day. An agency spokesperson did not immediately respond to a request seeking comment regarding the CMS approval.
The California Hospital Association, which lobbies for most of the state’s safety net hospitals that would also be impacted by the pending transition, did not respond to a request seeking comment.