Patients receiving inpatient care at 340B disproportionate share hospitals are significantly more likely to be low income than those receiving outpatient care, according to a new study funded by the brand name drug trade group PhRMA.
Hospital eligibility in the 340B program for disproportionate share hospitals (DSH), rural referral centers and sole community hospitals is partly determined by the institution’s DSH patient adjustment percentage, a reflection of a hospitals inpatient Medicaid and Supplemental Security Income (SSI) days. Free-standing children’s hospitals and free-standing cancer hospitals do not receive DSH funding. However, they must demonstrate that their inpatient mix would result in a DSH adjustment payment percentage of 11.75 or greater. A hospital with a DSH adjustment percentage of 11.75% translates into a patient population of close to 30 percent Medicaid or SSI inpatients. Critical access hospitals do not receive DSH funding and their eligibility is not determined by patient mix.
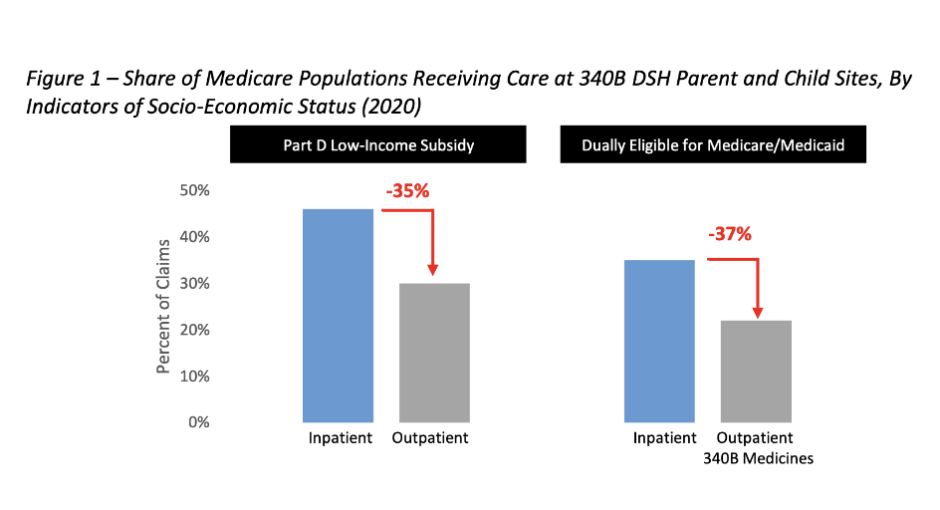
The study, conducted by the consulting firm ADVI, found that Medicare beneficiaries who were hospitalized at 340B DSH hospitals were approximately 35% more likely to have the Part D Low Income Subsidy (LIS) and to be dually eligible for Medicare and Medicaid coverage than were beneficiaries served on an outpatient basis who obtained 340B drugs from DSH hospitals and child sites.
ADVI researchers analyzed Medicare fee-for-service claims data from 2018 through 2020 to determine shares of Medicare beneficiaries with low income—indicated by LIS enrollment or dual coverage eligibility—served at DSH hospitals and/or child sites on an inpatient versus outpatient basis. Results are consistent across all years of data analyzed, researchers say, though only results from 2020 data are presented in the report.
“The significant difference between Medicare beneficiary demographics for inpatient and outpatient claims demonstrates that inpatient metrics—like DSH thresholds—may not be the most appropriate measure to determine covered entity eligibility for the outpatient-based 340B drug discount program,” the authors said.
Hospital Group Responds
Rather than undermining these hospitals’ eligibility for 340B, the PhRMA-funded study in fact “confirms the longstanding fact that 340B hospitals treat high numbers of low-income patients,” said Bharath Krishnamurthy, senior associate director of policy at the American Hospital Association. “Their own analysis shows that at least a third or more of 340B hospitals’ patients are low-income and reinforces the fact that the program is working to stretch scarce federal resources as far as possible, reaching more vulnerable patients—just as Congress intended when it created the program 30 years ago,” Krishnamurthy said.
The ADVI study was released within a day of a different one commissioned by 340B Health. The latter study found hospitals participating in the 340B program treat much higher shares of underserved patients than non-340B hospitals and physicians’ offices. The 340B Health study also examined demographic characteristics of Medicare beneficiaries over a similar timeframe, and, while it did not include LIS status, it did look at dual eligibility, as well as age, disability status, race, and ethnicity.
340B Health spokespersons could not be reached for comment on the ADVI study.