The state of Vermont has passed a bill extending its prohibition on discrimination by pharmacy benefit managers (PBMs) against 340B covered entities, which was originally passed in June 2021 as part of the state’s 2022 budget.
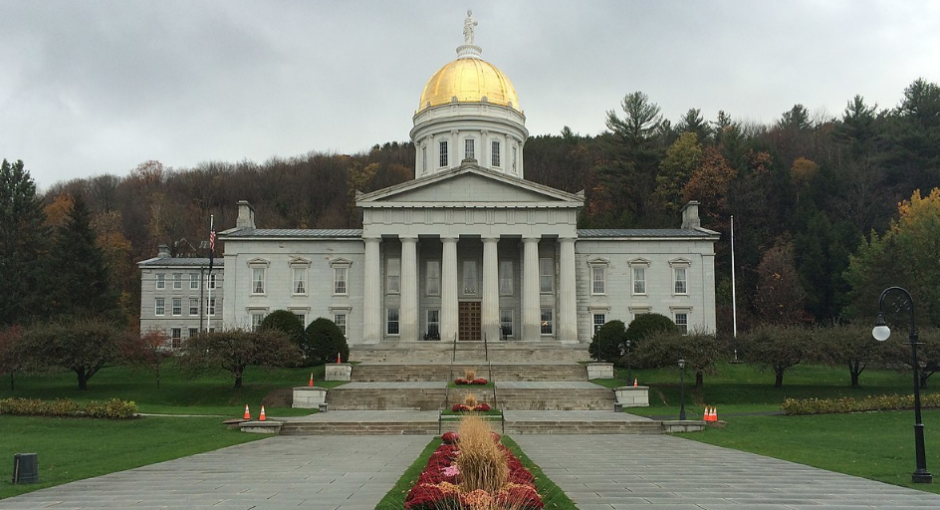
The bill was quietly passed by the Vermont legislature and signed into law by Gov. Phil Scott (R) on May 24, 2022. While covered entities and their advocates were able to extend and strengthen 340B protections in Vermont, they were not able to successfully add a provision to require drug manufacturers to provide 340B-priced drugs to contract pharmacies. Connecticut and California also recently attempted to prohibit manufacturers from imposing contract pharmacy restrictions but were likewise unsuccessful in getting these laws passed during the current legislative session.
Unlike the Connecticut and California measures that reportedly died due to last-minute drug company lobbying campaigns, the Vermont provision to protect 340B covered entities from drug manufacturer restrictions likely would have passed if not for concern among state attorneys involved in crafting the bill regarding how courts would define states’ rights to regulate manufacturer behavior in the 340B realm, according to Nathan Awrich, Vice President of Pharmacy Operations for the University of Vermont Health Network. These concerns led to the provision being pulled from the bill toward the end of the fine-tuning process, he added.
Arkansas enacted such a law in May 2021 and PhRMA has answered with a lawsuit alleging violation of federal preemption and the commerce clause. The case is currently pending in federal court in Little Rock. “I think what we’ll try to do is over maybe the next year or so, see how the litigation plays out, see how many other states pass similar laws, and then try to revisit it. Because there wasn’t really strong opposition, there was just concern around the risk,” Awrich says.
Updates to the Law
The original budget provision enacted in 2021 was intended as a “short-term fix” until more permanent, comprehensive legislation could be passed in Vermont, says Awrich. The provision was set to expire on January 1, 2023, but has been extended to April 1, 2024 under the recently passed legislation, which includes several other PBM-regulating provisions beyond those pertaining to 340B.
The 2022 bill (Act 131, H. 353) both maintains and enhances protections for 340B covered entities included in the budget provision passed in 2021 (No. 74, H. 439). The original legislation banned PBMs from requiring covered entities to add a modifier identifying 340B-eligible drugs when submitting claims for reimbursement—a practice known as “claims tagging”—and also prohibited PBMs from restricting pharmacy networks or adjusting reimbursement rates for contract pharmacies.
The new bill keeps both these provisions while adding two more that further elucidate and strengthen 340B anti-discriminatory protections. The bill forbids PBMs from reimbursing 340B providers at a rate lower than that paid to entities not participating in the 340B program, and from assessing “any fee, charge-back, or other adjustment on the 340B covered entity on the basis that the covered entity participates in the 340B program.” It also prohibits PBMs from discriminating against covered entities in a manner that would interfere with patients’ ability to obtain medications from them.
“While we need Congress to act, legislation like Act 131 emphasizes the value states place on the 340B program and the services it supports,” says Mary Kate Mohlman, Director of Vermont Public Policy for the Bi-State Primary Care Association representing Vermont and New Hampshire. “With the savings derived from the 340B program, FQHCs are able to provide Vermonters important services such as dental, nutrition, school-based care, transportation, translation, and discounts on prescription drugs, to name a few. However, efforts are being made to erode the program, thereby putting the availability of these services in jeopardy,” Mohlman says.
Opposing forces
Awrich says PBMs and other payers were the primary opponents of the legislation regulating their practices, but they were more concerned about the non-340B components of the new bill. However, some independent pharmacies and private physician practices in Vermont have “mixed feelings” about 340B, Awrich says
For independent physician practices, these feelings stem from “years and years of messaging,” from organizations such as the Community Oncology Alliance that characterize the 340B program as “a profit grab for hospitals, that leaves them to gobble up all of the independent practices,” Arwich says.
In the case of those independent pharmacies that do not participate in the 340B program, there is a general lack of understanding regarding 340B, says Awrich. However, the state’s independent pharmacy association’s enthusiastic support of “every other part of the bill,” meant that they were willing to let the 340B provisions remain, he says.