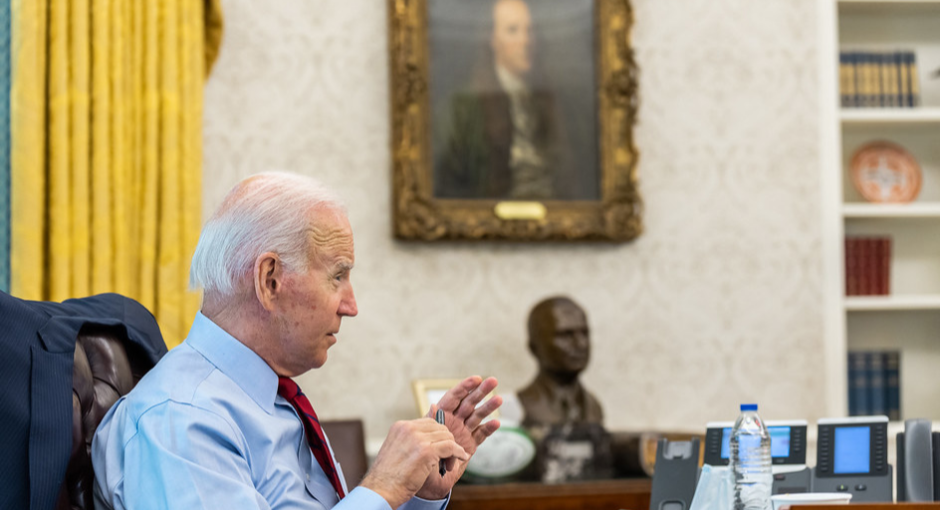
President Joe Biden this afternoon is scheduled to sign legislation that for the first time will let Medicare negotiate the prices of certain costly prescription drugs and require drug makers to pay Medicare rebates when their prices outpace inflation.
House Democrats returned temporarily from recess Aug. 12 to approve the Inflation Reduction Act of 2022 in a 220-207 vote along party lines. Senate Democrats pushed their version of the bill through via the budget reconciliation process on Sunday, Aug. 7.
The bill’s language cements price protections that 340B providers had pushed for, which enables 340B covered entities to access the lower of the 340B price or the “maximum fair price” negotiated by Medicare. However, the flip side is that, as Medicare bargains for lower prescription drug prices, that will result in smaller savings reimbursed to 340B providers.
The bill gradually increases the number of “negotiation-eligible” drugs cumulatively over time, with a total of 80 prescription drugs covered by Medicare’s new bargaining authority by 2030.
Specifically, the U.S. Department of Health and Human Services (HHS) can initially negotiate the prices of 10 top-selling, single-source Part D drugs, with the prices taking effect in 2026. HHS can then select 15 additional Part D drugs for negotiation, with the prices effective in 2027, then an additional 15 Part B or D drugs, with prices taking effect in 2028.
In the final phase, HHS can negotiate the prices on 20 additional Part B or D drugs, with prices effective in 2029, then 20 more drugs the year after.
The legislation sets criteria for selecting drugs that qualify for government negotiations, targeting Part B and D drugs that have cost Medicare the most money over the preceding 12 months. It also carves out exceptions, excluding drugs for which Medicare’s total spending is less than or equal to 1% of total outlay under Part D, new formulations of an eligible drug, and orphan drugs.
The negotiating power would result in government savings of $288 billion over 10 years, according to a Congressional Budget Office estimate.
The legislation also requires manufacturers to pay rebates on Medicare drugs reimbursed under Part B or D when the average manufacturer price for a particular drug rises faster than inflation, with the rebate calculated based on the difference between the drug maker’s price and the inflation rate for all sales of that drug to Medicare. The inflation penalty has been effective in tamping down prices in both the 340B and Medicaid rebate programs and the authors of the new Medicare law are hopeful that it will also play an important role in restraining prices for Medicare beneficiaries.
The bill includes language to protect a drug manufacturer from having to pay two inflation penalties on the same drug. This is done by excluding 340B purchases from the Part B and Part D rebate calculations.
The bill’s other key drug pricing provisions:
- Cap Part D beneficiary total out-of-pocket spending at $2,000 per year
- Cap premium growth at 6% per year through 2029
- Cap insulin costs for Medicare patients at $35/month
- Eliminate cost sharing for adult vaccines covered in Medicare Part D
- Expand income eligibility for Medicare Part D low-income subsidies
- Repeals Trump Administration’s drug rebate rule, requiring pharmacy benefits managers to pass on saving to patients at point-of-sale