UPDATE Tuesday, Oct. 26, 2021, 5:00 p.m. EDT—We have updated this article to reflect new information from the California Department of Health Care Services (DHCS) about the timeframe for the U.S. Centers for Medicare & Medicaid Services (CMS) to complete its review of DHCS’s Medicaid Section 1915 waiver. We also have added comment from the nonprofit group CaliforniaHealth+ Advocates.
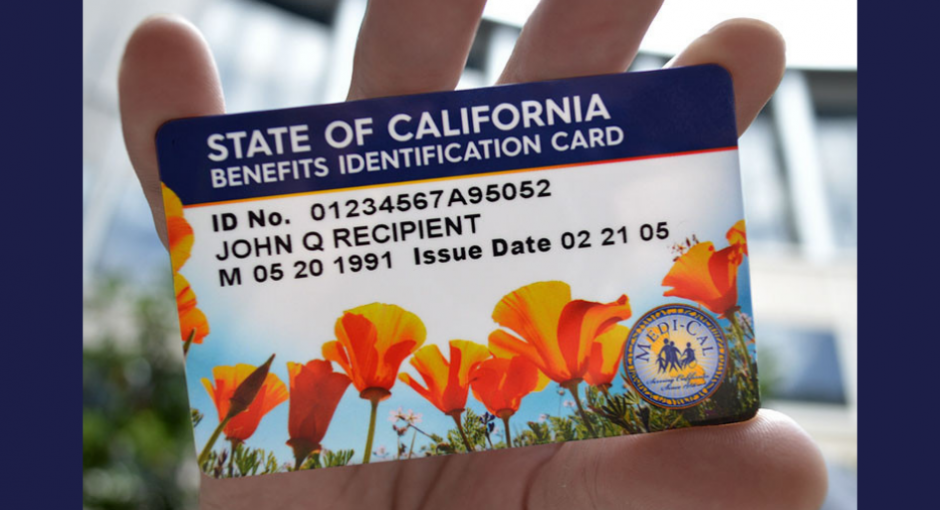
California’s Medicaid (Medi-Cal) program remains on track to move its pharmacy benefit from managed care to fee-for-service early next year, a change that would deprive federally qualified health centers and other safety net health care providers of hundreds of millions of dollars of revenue derived from the 340B program.
The shift is intended to save the state money in the administering of pharmacy benefits for Medi-Cal, a massive program in that insures 13 million California, or nearly one in three of the state’s residents. However, that would require covered entities to bill Medi-Cal at acquisition cost for all drugs they acquire through 340B, depriving them of critical revenue. Entities currently bill Medi-Cal FFS at acquisition cost for 340B drugs, but they bill Medi-Cal managed care organizations at higher negotiated rates.
Anthony White, president of the Community Health Center Alliance for Patient Access, (CHCAPA), said that the switch could cost covered entities between $200 million and $300 million a year in lost 340B revenue. Meanwhile, the switch is expected to save the Medi-Cal program no more than $175 million a year, according to documents obtained by White, who also serves as senior director of external affairs for Family Health Centers of San Diego.
“That cost is gradually increasing as well,” White told 340B Report, adding that numerous community health centers have become covered entities since the switch was first announced through an executive order by California Gov. Gavin Newsom (D) in January 2019.
New York State has undertaken a similar initiative, but it has been delayed until at least April of 2023.
Implementation in California was originally planned for the start of this year, but it was pushed back. The California Department of Health Care Services (DHCS) had announced on various portions of its website that the implementation will begin on Jan. 1, 2022.
According to new information today from DHCS spokesperson Anthony Cava, the new timeframe for the U.S. Centers for Medicare & Medicaid Services (CMS) to complete its review of DHCS’s Section 1915 Medicaid waiver application, which includes the prescription drug benefit transfer from managed care to fee for service, is Jan. 9, 2022.
“DHCS recognizes the important role of our safety net providers and the critical work they do for Medi-Cal beneficiaries,” Cava said. “DHCS engaged in stakeholder consultation in developing a 340B supplemental payment pool for qualified 340B clinics.”
CHCAPA is leading a group of 31 community health centers in a lawsuit originally filed against DHCS last year, but the litigation was dismissed without prejudice by a federal judge last March pending CMS’s final action on DHCS’s Section 1915 waiver application. CHCAPA will immediately refile the lawsuit if CMS approves the waiver, White said. CHCAPA would likely ask for a preliminary injunction against the switch, White said.
“We’re really hopeful because the case hasn’t really been heard at all,” White said.
Support for the switchover from managed care to fee-for-service is mixed outside of community clinics. Anthony Wright, executive director of Health Access California, one of the leading patient advocacy groups in the state, supports the change.
“We have supported the general push to consolidate the state’s prescription drug purchasing to drive a better bargain from the prescription drug companies,” he said in an email. “At the same time, we have supported a variety of patient protections to help ensure that consumers get the medications they need through the new process, and to ensure that the community clinics are held harmless in the switch.”
Although the state has authorized $100 million in supplemental payments to health centers during the first year of the transition, CHCAPA has maintained that sum won’t make up the shortfall.
CaliforniaHealth+ Advocates, an affiliate of the California Primary Care Association, is also deeply concerned about supplemental payment pool’s adequacy.
“CaliforniaHealth+ Advocates continues to prioritize making sure that health centers and the patients they serve are not harmed in this transition,” said Ayo Taylor, the organization’s associate director of strategic communications & public affairs. “We are still deeply concerned with financial impacts. This is why we are, and will continue to, push for an increase of the supplemental payment pool to guarantee no pharmacy has to close, no service or staffing is reduced.”