A new bipartisan bill to make insulin more affordable for patients could be up for a U.S. Senate vote as early as next month. There are doubts the bill will get enough Republican support to pass, however, dooming it to go the way of a recent string of failed drug-pricing bills.
Insulin has been at the heart of several recent 340B policy fights. Insulin and diabetes drug makers were among the first to impose conditions on the 340B contract pharmacy program. Three of those companies face antitrust charges over their contract pharmacy restrictions in federal district court in western New York State. The Biden administration rescinded a Trump administration rule requiring community health centers to pass along all their 340B savings on insulin to low-income patients with high-cost or no health insurance.
The U.S. insulin market was estimated at just over $20 billion in 2021, with roughly half of that attributed to Novo Nordisk products, and Lilly and Sanofi insulin drugs accounting for about one-quarter market share each.
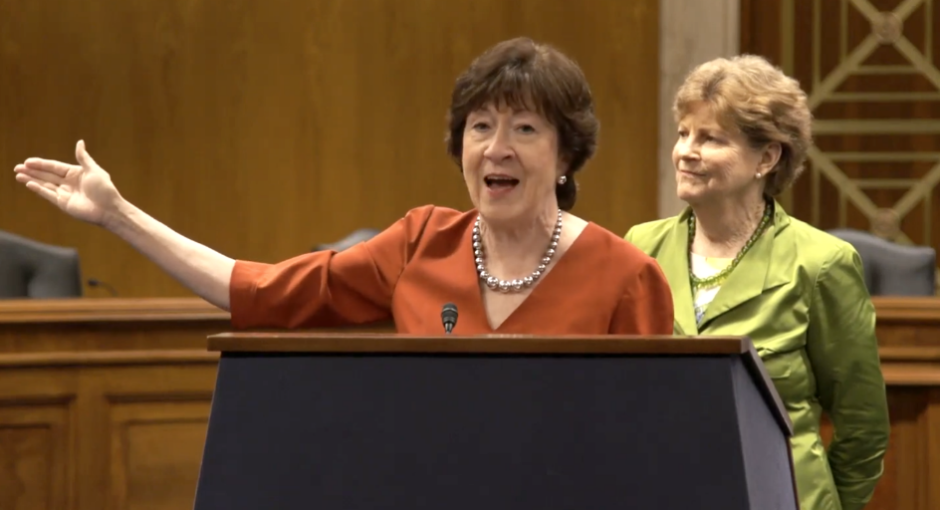
Senate Majority Leader Chuck Schumer (D-N.Y.) said last week he intends to bring the Improving Needed Safeguards for Users of Lifesaving Insulin Now (INSULIN) Act, co-sponsored by Sens. Jeanne Shaheen (D-N.H.) and Susan Collins (R-Maine), to the floor “very soon.” The Senate is on a two-week break now and is back in session on July 11.
According to a news release, the bill would incentivize insulin makers to reduce their list prices. Insurers and PBMs would be prohibited from getting rebates on insulins if manufacturers cap the list price to the 2021 net prices for Medicare Part D or equivalent levels. Such insulins would be eligible for cost-sharing protections, including a waiver of any applicable deductible, and limiting copays or coinsurance to no more than $35 per month or 25% of list price. The bill would support patient access by ensuring coverage and that prior authorization or other medical management requirements cannot be imposed to limit beneficiary use.
The bill also would require group and individual market health plans to waive any deductible and limit cost-sharing to no more than $35 per month, for at least one insulin of each type and dosage form.
Some patient advocacy groups say the bill is too soft on drug manufacturers, for example by allowing them to preserve their profits from 2021 onward.
Recent legislative efforts to rein in prescription drug prices have stalled. For example, a provision in the $1.75 trillion Build Back Better bill that died in the Senate last fall also capped insulin drug prices at $35 and required that Medicare Part D and private plans would have to cover all insulin products starting in 2025.
The House in November had passed a budget reconciliation bill that included major parts of H.R. 1, the drug pricing bill the House passed during the last session of Congress. However, Senate Democrats couldn’t get the 50 votes they needed to pass it and have since made a few unsuccessful attempts to bring watered-down drug pricing bills to the floor for a vote. But with the November midterm elections looming, time is running out with Congress in recess most of August, the first week of September, and most of October.
GOP lawmakers have been resistant to helping the Democrats accomplish a much sought-after win on drug pricing.