SPONSORED CONTENT
This strategy could save the 340B proceeds at your organization
Today, underinsured or uninsured patients who are undergoing treatment with a Gilead HIV treatment or preventative medication may be eligible to receive those medications at no cost through Gilead’s Advancing Access program. Under this program, covered entities are able to receive full 340B proceeds from these dispenses and can use these funds to support and expand critical community programs and outreach efforts.
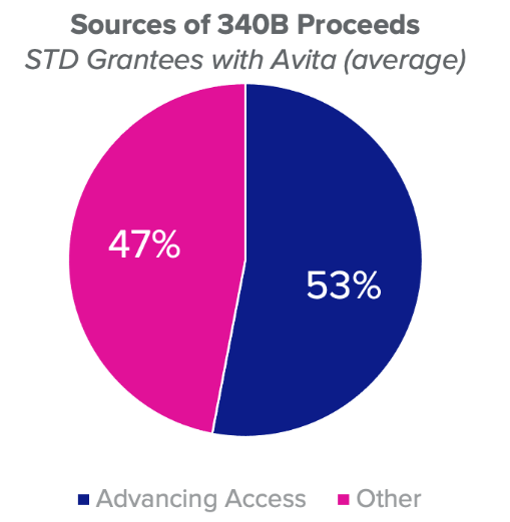
As most Ryan White and STI grantee covered entities probably are aware, on January 1, 2022, Gilead will no longer reimburse pharmacies at full retail price under its Advancing Access program. This will eliminate nearly all the 340B proceeds you may be currently receiving under this program and could have a huge impact on your business and the services you provide your community.
However, many covered entities or their patients may have not considered whether there may be other coverage options available to Advancing Access patients. These other coverage options could help patients secure quality coverage that can help ensure their access to HIV treatment or preventative therapies. These include coverage options in the marketplaces created by the Affordable Care Act. Many Advancing Access patients may find that they are eligible for significant federal premium and cost sharing support that could make their coverage very affordable. If patients elect to enroll in these programs, it could help mitigate the impact of the impending changes to the program.
Avita, in partnership with Pride Life LLC, has developed a customized solution for our contract pharmacy partners: the Avita Insurance Management Solution.
This solution focuses on helping Advancing Access patients consider whether they might be eligible to enroll in low cost, quality commercial health insurance. As a plus, this eliminates the dependency on Advancing Access while their prescriptions would nearly always remain 340B eligible.* Avita works with Pride Life LLC to identify plans that provide the best value and coverage to the patients and also works with covered entities and patients to enroll them in the plan. Many patients may find that these coverage options are very low cost, sometimes free. Avita provides customized reporting on patient adherence and actively monitors the value of the program to its provider partners to ensure that both patients and providers are benefiting from this arrangement.
If this is a strategy you are interested in for your covered entity, there is not much time left to make it happen. Open enrollment for the healthcare.gov and state exchanges is happening now and may end as early as December 15, depending on your state.

We know you won’t be ready to make any Insurance Management Solution commitments yet, and that’s ok. However, there is much we can do to put you in a position to be able to take advantage of this program if you so choose. We can actually get started with the HRSA registration without committing you to anything. Avita can even perform a custom assessment to see if this program can help your organization and your patients. We’ll walk you through the economics and show you the impact of the Advancing Access changes on a your 340B revenue.
If this is something you’re even remotely considering, I would love to speak with you. You can reach me directly at Glen.Pietrandoni@avitapharmacy.com and we’ll schedule a time to walk you through the process and answer any questions.
*Federal guidance from HRSA suggests that insurance premium assistance may be recommended for grantees. CE’s should consult their legal counsel before implementing any premium assistance program.
To learn about Avita’s CEO Michael Yount, see his 340B Leader Spotlight here.



