The U.S. Centers for Medicare & Medicaid Services starting Jan. 1, 2024, will require all 340B covered entities—hospital and grantee—to use claims modifiers to identify drugs as having been purchased through 340B when they bill for separately payable Medicare Part B drugs. In the meantime, it is encouraging entities to start using the modifiers “as soon as possible.”
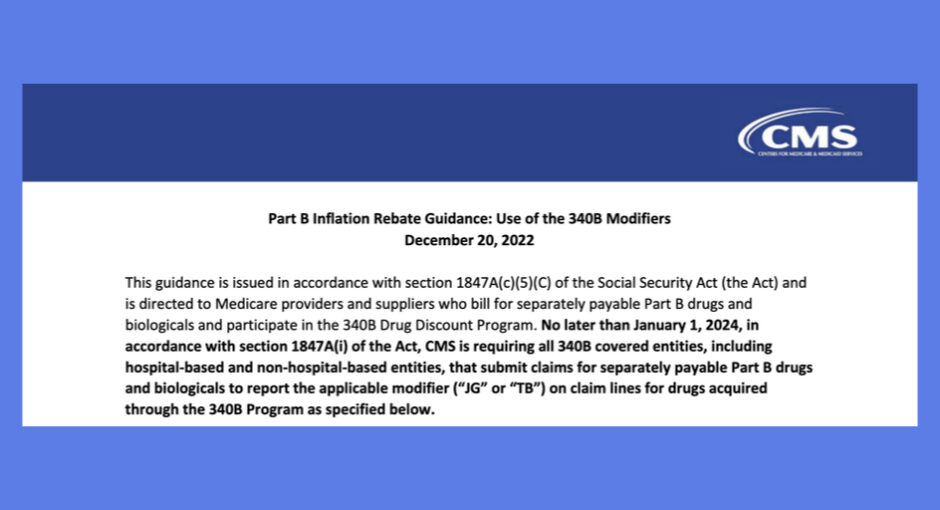
A CMS guidance document on the agency’s website dated Dec. 20 describes the new mandate. CMS said it issued the requirement to implement new Part B rebates manufacturers will owe Medicare when their drug prices increase faster that the rate of inflation. Manufacturers do not have to pay inflation rebates drugs sold at a 340B discount but will continue to be subject to an inflation penalty on non-Medicare drugs.
“Effective implementation of the Part B inflation rebate requires CMS to identify units of drugs acquired through the 340B program so they can be subtracted from the total number of otherwise rebatable units as applicable,” the guidance said.
Jan. 1 is the start of the first quarter during which drug manufacturers will be subject to the new rebates. CMS has until September 30, 2025, to invoice for rebates owed for quarters in 2023 and 2024.
Disproportionate share hospitals, rural referral centers, and non-rural sole community hospitals have been using the “JG” modifier since 2018 under CMS’s now-defunct deep cut in Part B reimbursement for the hospitals’ 340B-acquired drugs. Under CMS’s 2023 hospital outpatient prospective payment system final rule published last month, CMS kept the claims identification mandate in place for those hospitals in 2023 for informational purposes.
Since 2018, CMS has required children’s hospitals, free-standing cancer hospitals, and rural sole community hospitals, on an informational basis, to use the “TB” modifier to identify their 340B drugs billed to Part B.
“As such, the ‘JG’ and ‘TB’ modifiers provide an existing mechanism to identify drugs acquired through the 340B program that is familiar to most 340B covered entities paid under the OPPS, and this guidance does not change the requirements established in the OPPS final rule,” CMS said.
The guidance does not explicitly say that critical access hospitals will have to start using the TB modifier, too, if they bill for 340B-acquired physician administered drugs. CAHs are not part of the OPPS payment system.
One healthcare lawyer said this morning the guidance says unequivocally that “CMS is requiring all 340B covered entities” to use the modifiers, meaning including CAHs. Another however said whether CAHs are included “is a good question … [it’s] definitely an issue for which clarity is needed.” A hospital pharmacy executive said yesterday that while the guidance does not specifically say CAHs must begin using a modifier, “I’m assuming we have to do it.” The executive said implementing the requirement could be challenging and expensive.
Grantee covered entities that administer 340B-acquired drugs to patients and bill them to Part B will have to begin using the JG claims modifier. The guidance specifically mentions Ryan White clinics and hemophilia clinics.
“While these modifiers have been required and utilized by 340B providers paid under the OPPS since calendar year (CY) 2018, this requirement may be new for other 340B covered entities,” the guidance said. “As this requirement will require operational changes to billing systems for some 340B covered entities (and other providers and suppliers as applicable), CMS encourages these such entities to begin using the appropriate modifier as soon as possible, and no later than January 1, 2024.”
“Further program instruction on the Part B inflation rebate is forthcoming and will include information on how CMS will determine rebatable units during CY 2023 for purposes of determining the Part B inflation rebate,” CMS said.