The U.S. Health Resources and Services Administration midday yesterday and the 340B prime vendor Apexus this morning, in connection with the end of the COVID-19 public health emergency late last night, withdrew mostly identical 340B program FAQs about use of 340B drugs in hospital offsite locations.
In a related development, the U.S. Government Accountability Office yesterday released a report about a 2022 law that let some hospitals stay in the 340B program despite losing 340B eligibility for reasons related to the COVID-19 pandemic.
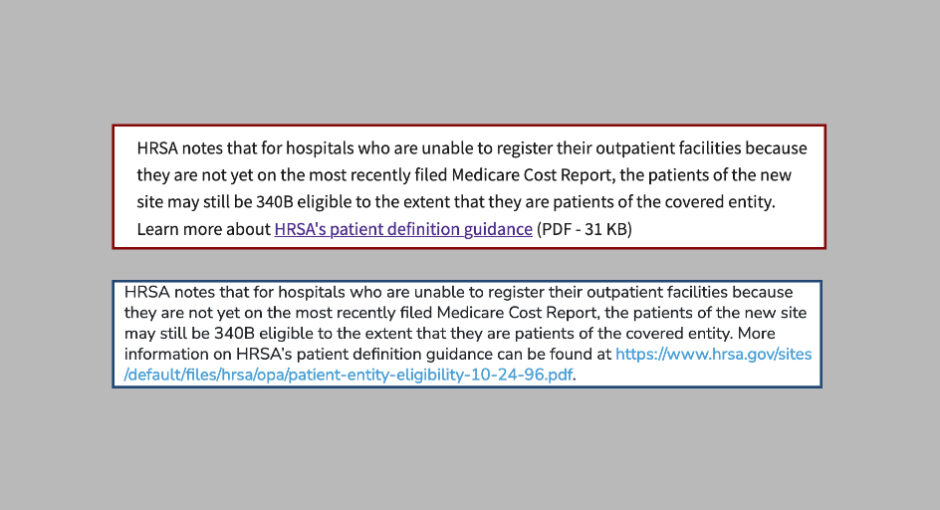
America’s Essential Hospitals urged HRSA in a letter yesterday to restore the policy that the withdrawn HRSA and prime vendor FAQs explained. The policy addressed 340B eligibility of hospital patients at offsite outpatient facilities not yet listed as reimbursable on the hospital’s most recent Medicare cost report.
The hospital group said that “the inadequate notice and lack of explanation for this change are unreasonable and inconsistent with requirements under federal administrative law.”
“For the benefit of underserved communities and the stability of the 340B program, we urge swift communication from HRSA clarifying that hospitals may continue using 340B drugs for eligible patients in offsite outpatient locations of the hospital that will appear on the next filed Medicare cost report,” America’s Essential Hospitals said.
Around noon Eastern yesterday, HRSA removed its 340B COVID-19 resources page from its website. The page included the FAQ about dispensing or administering 340B drugs to patients at hospitals sites not yet on the hospitals most recent cost report. HRSA told 340B Report in June 2020 that the policy the FAQ described was “in place regardless of the COVID-19 pandemic.” The prime vendor subsequently published an FAQ that was nearly identical. Its FAQ said nothing about the pandemic.
340B Report reported Monday that HRSA told it late on May 5 that “the flexibility that allowed hospitals to use 340B in offsite outpatient facilities not yet listed as reimbursable on a hospital’s Medicare cost report will no longer be available when the public health emergency expires.” Hospitals said the announcement was totally unexpected.
HRSA said yesterday in a note on the Office of Pharmacy Affairs home page, “Covered entities should continue to comply with the 340B program statute and all applicable regulations, guidance and policies. For audit purposes, entities should continue to maintain accurate records (including their policies and procedures) documenting their compliance with the 340B Program statute and all applicable regulations, guidance, and policies.”
“HRSA understands that the end of the PHE may raise questions regarding 340B program administration and compliance,” the note continued. “To the extent a 340B stakeholder has a specific circumstance where they believe the end of the PHE may affect their enrollment and compliance in the 340B program, the stakeholder should contact” the 340B prime vendor and it “will coordinate with HRSA, and each issue will be evaluated on a case-by-case basis,” HRSA said.
A HRSA spokesperson said late this morning, “HRSA’s website contains the most up to date information.”
New GAO Report
Meanwhile, the U.S. Government Accountability Office yesterday released a report, requested by the Republican chair of the House Energy and Commerce Committee and the previous Republican leader of the Senate Health, Education, Labor, and Pensions Committee about a 2022 law that let some hospitals stay in the 340B program despite not meeting a 340B eligibility requirement. The law let HRSA grant 340B eligibility exceptions to hospitals whose Medicare disproportionate share adjustment percentage fell below the level needed to stay in 340B due to factors related to the COVID-19 PHE.
GAO said 61 hospitals requested an exception as of May 31, 2022. Of those, 53 were approved and eight were denied. It said in a footnote that 94 hospitals requested an exception as of January 31, 2023. Of those, 82 were approved (including 13 hospitals that received a second exception) and 12 were denied. The report focuses almost entirely, without explanation, on the 53 that got exceptions.
Of those 53, 33 DSH hospitals, 14 sole community hospitals, and six rural referral centers got exceptions. GAO said most of the hospitals were rural (35) and had 100 or fewer beds (31).
The DSH percentages of the 53 hospitals ranged from 0.2 to 9.0 percentage points below their required DSH percentage thresholds for 340B eligibility. Some hospitals said state moratoriums delaying elective procedures were to blame.
Thirty-three of the 53 hospitals “consistently operated with a positive total facility margin in each year from fiscal years 2017 through 2020,” GAO said. “Most hospitals saw year-to-year fluctuations—both increases and decreases—in the amounts of charity care, uncompensated care, and total unreimbursed and uncompensated care they provided as a percentage of total facility revenue,” it said. Most saw year-to-year fluctuations—both increases and decreases—in their DSH percentages from 2017 through 2020.
The amount that excepted hospitals reported paying for 340B drugs varied considerably, GAO said, ranging from about $42,000 to about $70.9 million in 2021 for the 39 hospitals that gave GAO complete payment data for that year. The median amount paid for 340B drugs was about $6.9 million.
“Based on excepted hospitals’ estimates of what they would have paid to purchase drugs if not participating in the 340B program in these years, the median discount percentage that the hospitals received on the 340B drugs they purchased was 42.4% in 2020 and 43.5% in 2021,” GAO said.
GAO sent hospitals that got exceptions a questionnaire during fall 2022 in connection with the study. Forty-eight responded. Of those, 30 reported having one or more active contract pharmacies that dispensed 340B drugs at the time they responded to the questionnaire. Of the 30, 16 reported providing discounts to low-income, uninsured patients at some or all of those pharmacies, GAO said.
Of the 48 that responded to the questionnaire, 23 reported having one or more in-house pharmacies that dispensed 340B drugs for patients’ home use at the time they responded to the questionnaire. Of the 23 hospitals, 19 reported providing discounts to low-income, uninsured patients at some or all of these pharmacies, GAO said.
Hospitals that responded to the questionnaire said participating in 340B let them provide services including:
- expanding chemotherapy infusion clinics, without which patients would have to travel long distances—often to another state—to receive care
- adding primary care providers in their service area or retaining specialists to provide care in rural areas
- conducting outreach to underserved communities, such as providing annual influenza vaccinations, COVID-19 testing and vaccination events, and health and wellness education
- providing mobile charity care to community members who are unhoused or living in rural areas.
“Some hospitals reported using 340B savings to offset costs or financial losses, thus indirectly benefiting their patients and communities by keeping the hospitals operational,” GAO said. “For example, one excepted hospital noted that savings from the 340B program helped it to absorb shortfalls from Medicaid reimbursements and other programs for low-income patients. Another hospital said its 340B savings feed into its overall operating budget, which helps keep its hospital afloat. A different hospital reported that the 340B program allows it to keep clinics open that may otherwise be too costly to maintain.”
GAO said HRSA as of July 2022 had audited 25 of the 53 hospitals that got exceptions. HRSA issued a total of 19 adverse finding to 14 hospitals. Five hospitals has more than one adverse finding. All 14 submitted corrective action plans.
The report said according to HRSA, “no drug manufacturers have requested to audit any of the 53 hospitals in our review since the beginning of the 340B program in 1992.”
Ten of the 53 hospitals had self-disclosed a total of 11 340B non-compliance events to HRSA as of July 2022, GAO said.
The report noted in passing that there were more than 2,600 hospitals in the 340B program as of January 2023.