Pennsylvania health centers are upset about what they say was the state Medicaid office’s disclosure without warning last week that, starting July 1, it wants drug claims billed to Medicaid managed care organizations to include a modifier showing if the prescription was filled with a 340B-purchased drug. The Medicaid office says the change is needed to stop drug manufacturers from being improperly invoiced for rebates on 340B-purchased drugs.
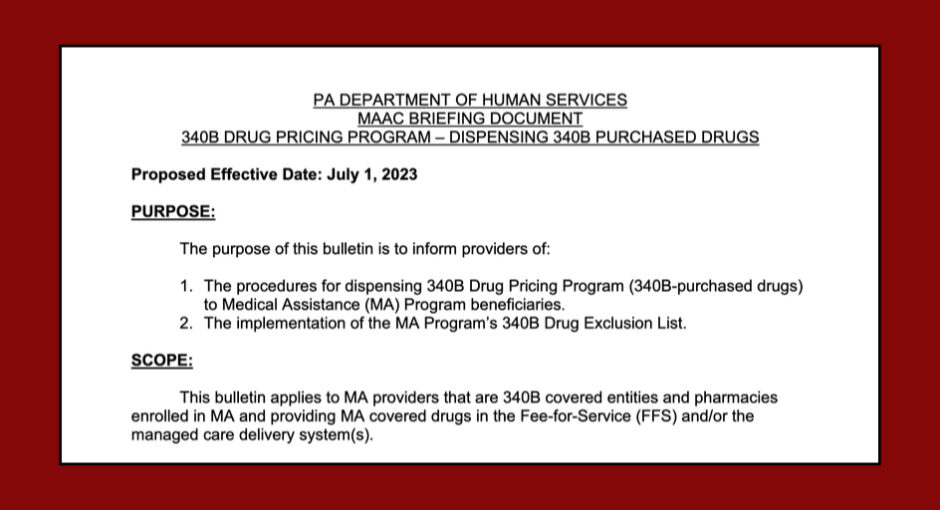
Health centers say if the state implements its proposed requirement, they effectively will be unable to dispense 340B-purchased drugs to Medicaid MCO beneficiaries, leading to major revenue losses and cuts in patient services. Pennsylvania Department of Human Services officials are scheduled to brief the state Medicaid advisory committee about the proposed change during a committee meeting Thursday.
Eric Kiehl, director of policy and partnerships at the Pennsylvania Association of Community Health Centers, said his group “has concerns that this briefing document outlining a proposed DHS strategy does not reflect the recommendations of” a 340B stakeholder workgroup that the state Medicaid office assembled early this year to seek consensus on how to prevent 340B duplicate discounts in the Medicaid managed care setting.
Kiehl said the state’s proposal as drafted “could create significant challenges to utilization of contract pharmacies in 340B. We appreciate the state’s commitment to ensuring 340B savings remain with the covered entities where they can be utilized locally to continue the essential services they support in underserved communities and for vulnerable populations. We look forward to continuing to work with the department to define and refine a solution that allows covered entities and the patients they serve to continue to benefit from this essential program designed to support them.”
The Hospital and Healthsystem Association of Pennsylvania was asked for but has not yet issued comment about the state’s proposal.
Pharmacy benefit manager Express Scripts caused an uproar in early 2021 when it announced a similar claims modifier requirement for 340B-purchased drugs dispensed by contract pharmacies. Noncompliance reportedly is widespread. Covered entities said under such policies, when a previously submitted claim is determined to be 340B-eligible, the burden is on contract pharmacies to resubmit the claims with the required modifiers. Entities said most contract pharmacies either cannot or will not comply, which means the prescriptions are filled with drugs purchased at above the 340B ceiling price.
New York state and California are preventing 340B duplicate discounts in the Medicaid managed care sphere differently—both shifted Medicaid managed care pharmacy benefits into Medicaid fee for service. Under Medicaid FFS, covered entities may not use contract pharmacies to dispense 340B-purchased drugs. For in-house pharmacies, they must choose between using or not using 340B-purchased drugs for Medicaid beneficiaries (carving in or carving out). If they carve in, the federal government lists them in the federal 340B Medicaid Exclusion File, the official data source to help prevent duplicate discounts in Medicaid FFS.
Without Warning Again, Entities Say
This is the second time in five months that the Pennsylvania state Medicaid office has made an announcement without warning about 340B duplicate discount prevention, covered entities say.
In late December 2022, the office gave providers about one week’s notice that, effective Jan. 1, contract pharmacies would have to dispense non-340B-purchased drugs to Medicaid beneficiaries in both Medicaid fee for service and managed care. “All drug claims paid to these providers will be invoiced to drug manufacturers for Medicaid rebates,” the office said.
The office rescinded the policy switch on Jan. 19 amid strong opposition from the state community health center and hospital associations. The state Medicaid office early this year began a series of meetings with covered entities and contract pharmacies to try to find a solution that all could live with.
Covered entities said the state was urged during those meetings to embrace a retroactive 340B claims identification process like Oregon’s to protect drug manufacturers from paying duplicate 340B discounts and Medicaid managed care rebates on the same products. Under that state’s method, 340B covered entities must tell the state, within 30 days of the end of a quarter, which drug claims they submitted to Medicaid MCOs during the quarter that they filled with 340B-purchased drugs. Oregon’s Medicaid rebate vendor then compares the data that comes from the covered entities with the original paid encounter data and excludes matching claims from rebate requests to manufacturers.
Providers said they were blindsided when the state Medicaid office last week, in advance of the April 27 Medicaid advisory committee meeting, released its draft requirements for dispensing 340B-purchased drugs to Medicaid beneficiaries.
A Pennsylvania health center 340B program director pointed out that the state’s proposed modifier requirement would apply to claims for 340B-purchased drugs dispensed to Medicaid managed care beneficiaries not just by an entity’s contract pharmacies, but by an entity’s in-house pharmacy too.
The health center 340B program director also observed that the proposed requirement says, “The 340B covered entity ensures that 340B claim identifiers are included only on claims
for 340B purchased drugs.” As a practical matter, there is no way for an entity to give such an assurance because the contract pharmacy, not the entity, adds the modifier, they said.
“We don’t have access to their software,” the person said, “we have no way of knowing that.”