SPONSORED CONTENT
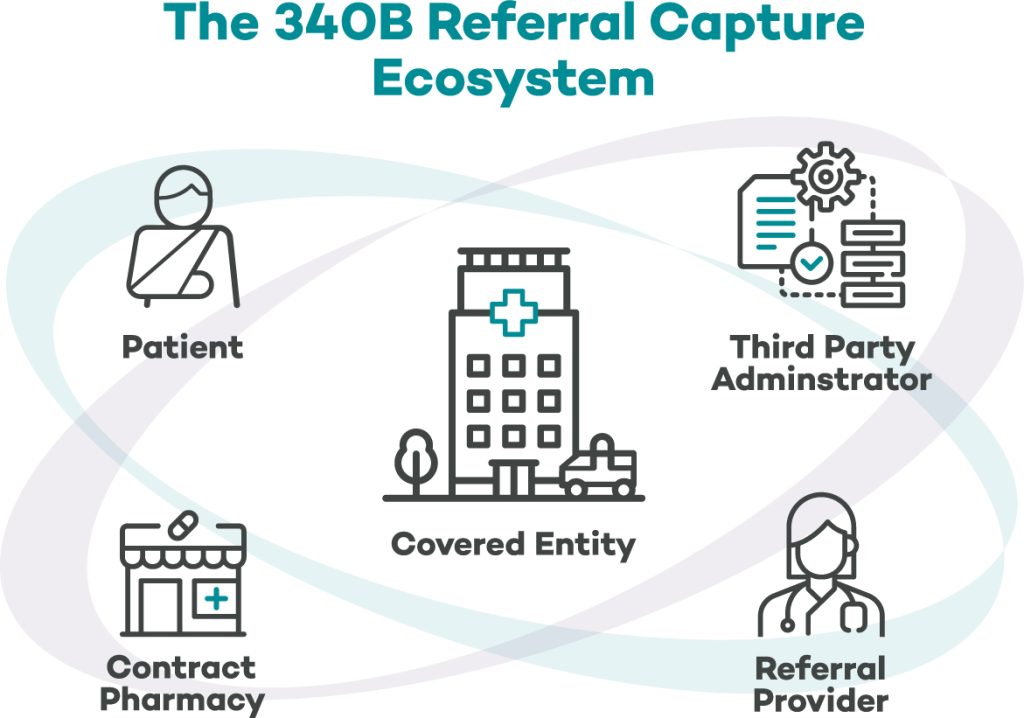
Referral prescriptions can be a critical source of 340B savings opportunity for covered entities (CEs) in their mission to “…stretch federal resources as far as possible, reaching more eligible patients and providing more comprehensive services.” Whereas only a few years ago CEs were reluctant to engage in referral prescription opportunities due to compliance concerns, many have since added referral prescription capture to their 340B programs and become more confident in how they have created additional value for their program.
Maintaining data integrity across all the partners that support a 340B program is a top priority for covered entities, which poses a risk for both noncompliance and variances in value performance if data about patients and/or providers becomes inconsistent or changes structure. The following are three key considerations to look for when analyzing potential opportunity in referral prescription capture.
1. The Right Contract Pharmacy
Contract pharmacies are an effective extension of 340B providers in providing prescription access and other healthcare services to eligible patients, highlighting the importance of selecting the right contract pharmacy partner to realize higher per-claim savings.
Understanding where patients are receiving a pharmacy service is a great targeting exercise for CEs to determine the best-fit with an external pharmacy. Utilizing the EHR is key to performing this exercise accurately because those systems support the reporting of outbound prescription orders to provide either a destination pharmacy (if electronically prescribed) or a patient’s preferred pharmacy. Many 340B teams may not realize they can access and utilize this data source, and leveraging this data is a key approach to understanding potential value.
Additionally, a contract pharmacy’s transparency in their forecasting methodology (e.g., how they calculate Medicaid-eligible populations) and ability to share and evaluate data with your referral management solution can influence per-claim savings:
- Thoroughly vet any promises of returns by qualifying assumptions made in the forecasting process.
- Have contract pharmacy partners describe what data they make available to covered entities and their affiliates to identify missed opportunities.
- Ask whether they have preferred data sharing relationships that you should consider as part of the selection process.
2. Patient Activity
Securing the documentation to support the patient’s referral episode of care is critical to meeting HRSA expectations about managing referral prescriptions. Some CEs that manage referrals on their own do not have great documentation workflows or have limited staffing resources so only focus on high-yield claims or targeted clinical service lines. Most vendors that advertise referral management services lack the direct integration with medical records systems and pharmacies to accurately identify referral opportunities in an automated fashion.
In contrast, a comprehensive solution should have both interconnectivity with your electronic health records and the contract pharmacy. This would allow it to automatically pair adjudicated prescriptions to outbound referral events and populate a queue of potentially eligible referral prescriptions. This results in a list of potentially eligible claims that are targeted to avoid ‘carpet bombing’ external providers and becoming a nuisance to their patient care efforts.
Another thing to consider when analyzing a patient’s referral episode of care is the range of time between the most recent encounter dates at both the CE’s and the referral provider’s offices. The frequency of how often a patient must visit a primary care service is not mandated by HRSA, and CEs may use discretion in developing a policy consistent with the needs of their population. For example, the National Association of Community Health Centers suggest that many health centers consider a patient ‘active’ if they have a visit within the past two years, as this practice is consistent with UDS requirements that patients been seen within the same timeframe. Additional factors that may be considered include the frequency for which recommend visits should occur in patients with chronic disease.
Evaluating the inclusion and exclusion parameters within a referral management solution can have a significant effect on the yield of eligible claims. Ensure that you are fully knowledgeable in this area and vet any programmatic changes with legal counsel as well as your compliance consultant if you have one.
3. Location and Provider Indexing
A major administrative burden for CEs is identifying their employed or contracted providers when third-party administrators are enumerating contract pharmacy claims. This is especially the case when maintaining a list of eligible locations.
Covered entities are susceptible to errors of omission when identifying all potential encounters and order types that may generate eligible prescriptions. Also, they may not be made aware of new units and departments that are stood up to address emergent clinical needs such as overflow units.
For current Cloudmed client partners, the 340B Recovery platform delivers multiple activities to identify and publish potentially eligible claims for which technology cannot wholly solve. The audit-first, technology-enabled service looks to capture ineligible scripts written by providers inside and outside one’s organization, in the form of ineligible claim and referral capture, and turn them into recovered 340B savings. And because Cloudmed’s Recovery platform provides the referring provider and supporting staff with easy access to specialist consult notes, Cloudmed fundamentally improves patient care coordination and continuity.
Our 340B experts can recommend adjustments and improvements to maintain ongoing compliance with 340B program requirements and identify opportunities to optimize program participation and savings. Learn more about Cloudmed 340B Recovery or schedule a meeting to talk to our experts today.

Donald Holladay, PharmD, 340B ACE, is Regional VP of Business Development at Cloudmed, an R1 company. He can be reached at Donald.Holladay@cloudmed.com.




